
It’s your first dayshift in a long time, but the overtime opportunity was a no-brainer. You and your partner hop in the rig and hit the road to grab early morning coffee at your local coffee spot down the street. Just as the barista hands you the steaming fresh pour-over the tones drop, the dispatch is for a 36-year-old female complaining of chest pain with shortness of breath. You hop in the rig, check the address, and find it conveniently two blocks down the street. You grab two quick sips of coffee and then make your way to the office park.
Gathering your equipment, you head to the main entrance and are greeted by security. They escort you and your partner to the elevator and take you up to the sixth floor. The doors open to another security officer who escorts you to a large meeting room. You can see through the glass windows a group of individuals huddled around a younger female seated but breathing fast and looking pale.
You walk up and calmly move all of her coworkers away as you kneel down. You shake her hand and introduce yourself. She says “hello” (in a struggling choppy tone), and that her name is “Sarah………. Mills.” As she looks you in the eye, you see the struggle on her face and hear her fatigue just getting those three words out.
Read: Friday Night Lights: Shift 1 – Balloons Under Water
You ask when this started and how she feels and she follows with “all…….of…….. the…… sudden.” Her coworker Tom jumps in to help answer questions as it’s clear she can barely get a word out. Tom says they were in the middle of a high-priority meeting about a security asset client when Sarah suddenly turned to him and said she couldn’t breathe and her chest hurt.
You gesture to your partner to get her hooked up while you hop up to talk with Tom so you do not increase Sarah’s work of breathing with more questions. You ask him what time she arrived at work, if she has any medical problems, did he notice anything different today, and how was she this morning? He tells you she’s healthy and runs regularly, got in early to get the documentation ready for today’s meeting and had no other complaints.
She joined the team for coffee before the meeting and he didn’t notice anything was off. You ask about the meeting and if there was anything he could think of that would trigger her symptoms. He said the meeting was about two hours in and was going well. You ask your partner to get bilateral blood pressures and a 12-lead EKG.
Your partner confirms the request and states she is going to put Sarah on supplemental oxygen via nasal cannula at 5 LPM based on her SpO2. About a minute later, your partner elbows you to look at the monitor.
You turn and see the below, is there anything jumping out at you? Is there any other test you want? What are your primary concerns?
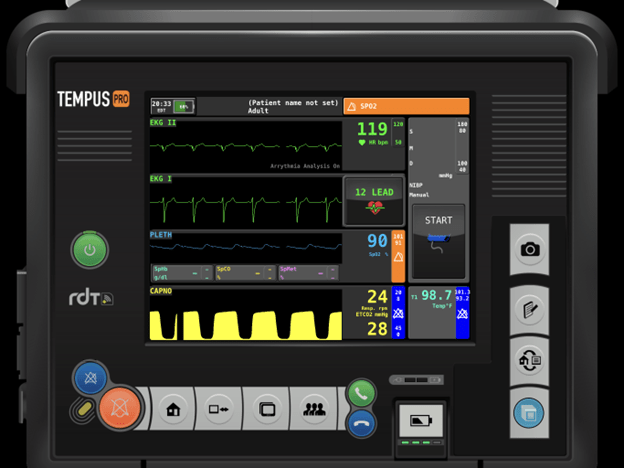
Looking back at the monitor and a couple things should jump out at you including sinus tachycardia, a lower-than-normal pulse oximetry, an increased respiratory rate and low EtCO2. Your brain starts creating a list of differential diagnoses that Sarah could be experiencing. Now you need to start breaking down and organizing your findings so you can figure out the differential that fits this pattern, presentation and rapid onset.
Sarah developed a sudden onset of shortness of breath and chest pain localized to the mid-sternum. She states it radiates to her back and she has a difference of 20 mmHg in her bilateral blood pressures. Analyzing these findings can help guide you to the potential of an upper aortic dissection. She’s an otherwise healthy female that all of the sudden had the signs and symptoms develop.
Read: Friday Night Lights: Shift 2 – Leaky Hose
When thinking about the pathophysiology of a disease process, you need to consider things that move or migrate, shear, rupture, or spasm rapidly versus delayed or progressive onset. What are some of the other things that fit with a sudden onset in a person who is tachycardic, mildly hypoxic, and with a low EtCO2? Your list of differentials should include pulmonary embolism which come in different sizes, variations and locations. A blockage in the pulmonary vasculature inhibits the body’s ability to bind oxygen to red blood cells and offload CO2 to the lungs.
Imagine a disabled vehicle blocking a one lane road, no red blood cells can get in to drop off their CO2 or pick up more O2. This causes a decrease in oxygenation, an increase in CO2 in the blood, and a reduced exhaled EtCO2. The body’s response to this is to ramp up the sympathetic nervous system. This increases circulation by raising the heart rate while simultaneously increasing respirations to potentially drive in more oxygen. When you see a person who has developed sudden onset of shortness of breath and/or chest pain, pulmonary embolism should be high up in your differential list. Add tachycardia, tachypnea, hypocapnia, and hypoxia, to chest pain and shortness of breath and PE should jump to the top of your list.
Your differential list might have initially and rightfully included panic attack. A high stress board meeting about a high stress client could easily trigger a panic attack. But after further investigation it doesn’t fit. What didn’t you see in Sarah that you would expect with a panic attack? Typically, panic attacks cause hyperventilation syndrome resulting in low PaCO2 or blood CO2. The hyperventilation blows down their CO2 and causes arterial vasoconstriction. This results in carpel spasms, periorbital tingling, ringing in the ears and lightheadedness.
Patients experiencing panic attacks shouldn’t have is a low SpO2 reading in the presence of a good pulse ox pleth wave. You may see artificially low SpO2 readings because the carpal spasms worsen blood flow to the fingers decreasing the accuracy of the probe reading. Always look at your pleth wave before acting on a value. If the pleth wave looks like VFib, the signal quality is poor and the number you’re getting isn’t accurate.
Not all pulmonary embolisms are the same. They come in different shapes, sizes and locations.
This means not every PE causes a person to pass out or code the minute an emboli lodges in their pulmonary vasculature. They also all don’t present with a blue collar around their neck or a blue head. These commonly referenced signs are only seen in the extreme saddle branch cases. Many patients, even those with large PEs are asymptomatic or have mild, non-specific symptoms.
Read: Friday Night Lights: Shift 3 – Above the Baseline
You reevaluate the severity and opt to hold on the EKG to get her onto the cot, and start working out to the unit. You let her coworkers know you are transporting to Memorial Hospital. En route you establish IV access and perform serial EKGs. You find the following:
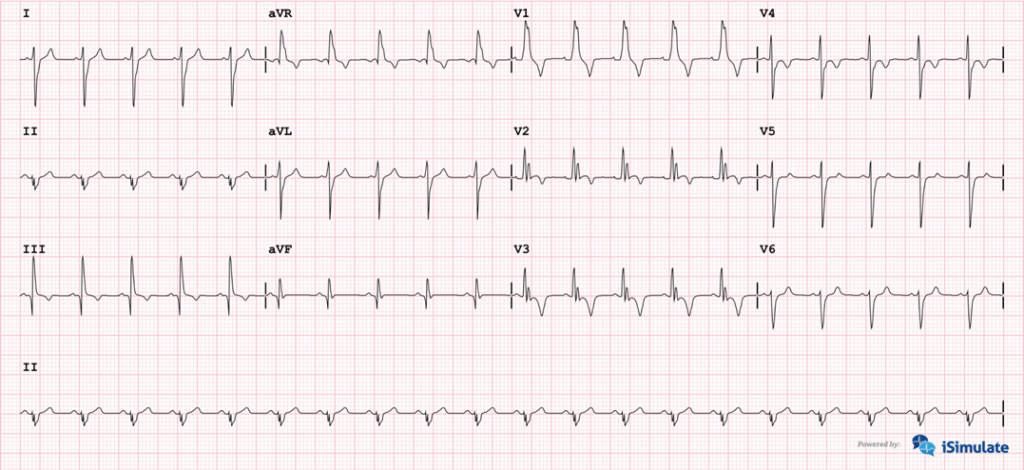
The most common EKG pattern in PE is sinus tachycardia.
Depending on size and location you may see a right ventricular strain pattern (S1, Q3, T3) on the EKG (see above). That is a deep prominent S wave in Lead 1, prominent Q wave in Lead 3 and T-wave inversion in Lead 3. This however is not specific to PE and can be seen in right heart failure as well (cor pulmonale).
Read: Friday Night Lights: Shift 4 – Wearing Off and Waking Up
Sarah has no other changes en route and you go right into bed three on arrival.
Chris Kroboth has been a career paramedic/firefighter for over 17 years and in EMS for over 23. He has been in prehospital and in-hospital education for the past 18 years. His last assignment before returning to operations was as the EMS training captain in charge of continuing education programs and certification. He is also affiliate faculty with the Virginia Commonwealth University Paramedic Program. He is the U.S. clinical education manager for iSimulate and also facilitates national conference clinical challenges to include EMS World, ENA and NTI.


Recent Comments