On the go? Listen to the article in the player below!
You and your partner are savoring the last drops of the best brew from the local coffee shop when the tones drop for a seven-year-old female with shortness of breath. It’s only about two miles away at the urgent care; as you start down the road, you bounce ideas back and forth with your partner. What are some of the things you think could cause this?
It’s winter, about four inches of snow remain on the ground from a snowstorm two days ago, and the temperature is 28 degrees Fahrenheit. Your partner backs into the ambulance parking spot at the urgent care. You hop out of the rig, grab your monitor and jump bag, and head inside. The staff directs you to room six where Emma James is sitting upright on the patient table, fixing and following you and your partner when you walk in. She’s breathing fast and shallowly with both hands on her knees. You’re greeted by the physician’s assistant (PA), discussing treatment with the mother. Emma developed some shortness of breath and chest discomfort two days ago that has progressively worsened. After being triaged, she was taken to the room and put on a non-rebreather mask. You smile and shake Emma’s hand, introducing yourself and letting her know you will take good care of her. With a smile, you tell her, “I just need to talk to mommy and the PA for one second.”
Read: Friday Night Lights: Shift 1 – Balloons Under Water
You also let her know your partner will hook her up to the monitor, get her vital signs, and confirm with her that it’s OK. She nods yes, eyeing your partner and the monitor. After discussing the findings with the PA and mom, you return to Emma and ask if she still has trouble breathing and chest discomfort; she nods yes. You glance at your monitor and notice the below vital signs. What jumps out at you? Is there anything of concern?
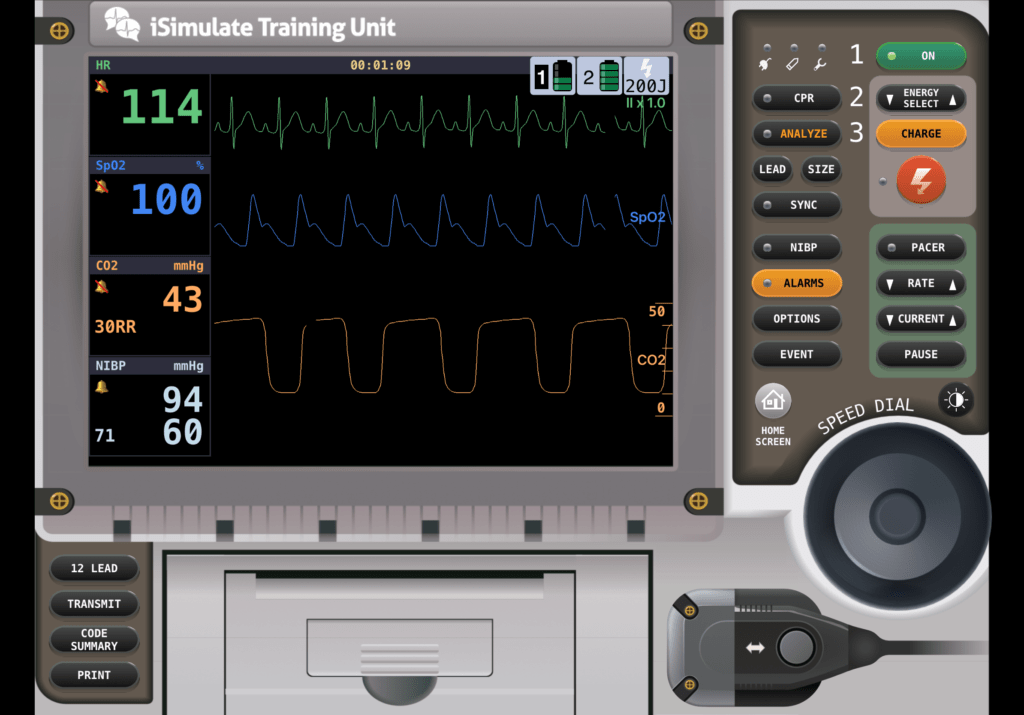
The only thing that seemed significant from the PA’s assessment was that Emma has a low-grade fever of 99.8 degrees and a mildly productive cough with dark yellow sputum. You ask mom if anybody else has been sick in the home. She says her husband recently got over a respiratory infection, and then she says there’s been a sickness going around Emma’s school, but she’s unsure of the symptoms. You glance back at the monitor, ask your partner to get lung sounds, and ask Emma if she feels better or worse than when you first arrived. She shrugs her shoulders. You direct your attention back to the monitor. You notice her heart rate is sinus tachycardia with no ectopy, her blood pressure is within the expected range for her age, and the SpO2 value and pleth wave look good. You turn to your partner and ask what the lung sounds are. Your partner states she heard gunky lung sounds on the right side and clear on the left side. She asks you to confirm; you take a listen and hear the following:
What are your differentials so far? And is there anything on the monitor that doesn’t look right?
Read: Friday Night Lights: Shift 2 – Leaky Hose
Let’s take a closer look at the capnography waveform.
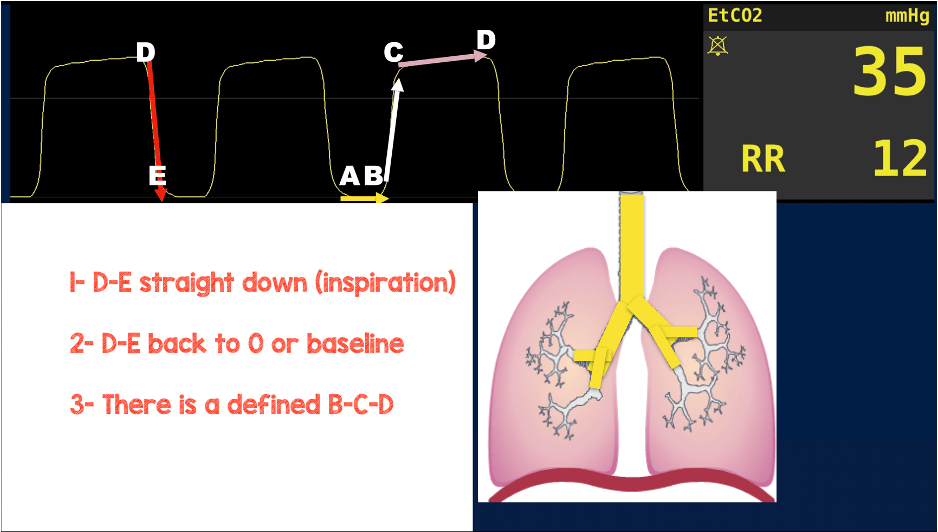
- Do you like the inspiratory phase?
- Does it go back to baseline?
- Does it have a defined B to C and C to D phase?
You notice it looks OK but doesn’t return to baseline at the end of the D to E phase. Why? What does this mean? Is it significant?
If the waveform does not return to 0 or baseline at the end of the D to E phase, it indicates rebreathing of the previously exhaled gas. Residual CO2 at the end of inhalation is elevating the baseline. There are a couple of things that can cause rebreathing. The first is a faulty exhalation port or valve, most commonly seen when a patient is on a ventilator or, less typically, on a BVM. It can also happen when a patient breathes fast with a mask on their face. The mask prevents CO2 from completely clearing the previously exhaled gas around the mouth and nose before their next (coming quickly due to rate) inhalation. The fix is simple. Just lift the mask and allow the air to purge, and their EtCO2 should return to baseline. You may need to do this intermittently until their breathing slows.

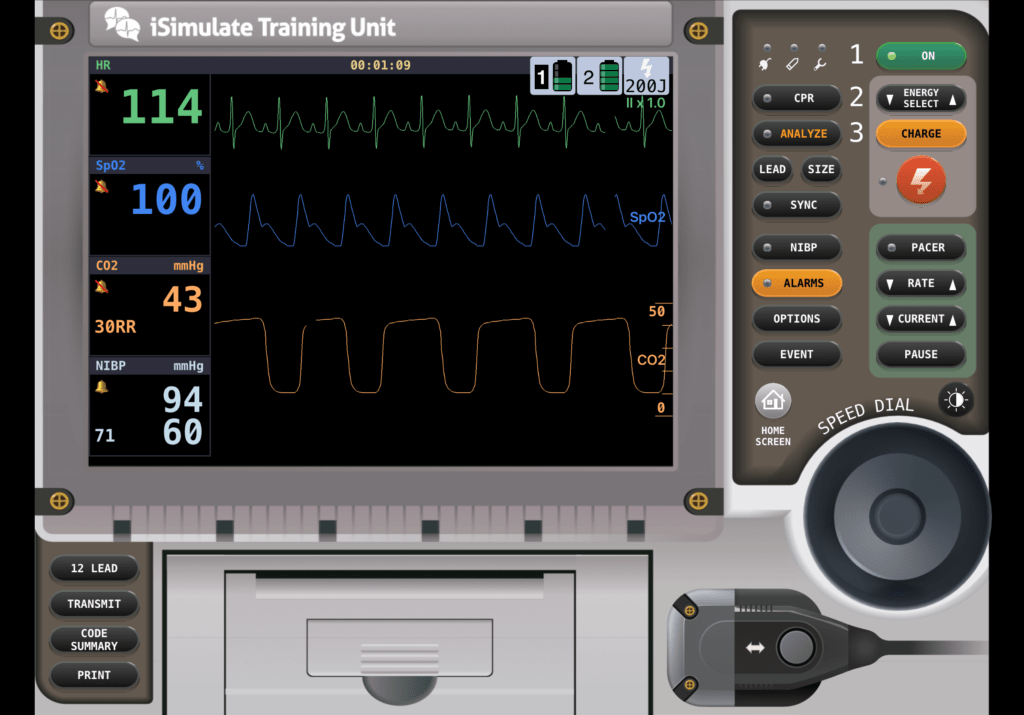
You lift the mask off of Emma’s face and notice the below. What do you think?
Now that we have cleared the exhaled CO2, the end-tidal has returned to baseline. You can now use the values you are getting on the capnograph. This example illustrates how capnography can be used to manage ventilatory quality and how interventions (in this case, a mask) are working or indicate a change in the patient’s status.
Chris Kroboth has been a career paramedic/firefighter for over 17 years and in EMS for over 23. He has been in prehospital and in-hospital education for the past 18 years. His last assignment before returning to operations was as the EMS training captain in charge of continuing education programs and certification. He is also affiliate faculty with the Virginia Commonwealth University Paramedic Program. He is the U.S. clinical education manager for iSimulate and also facilitates national conference clinical challenges to include EMS World, ENA and NTI.


