
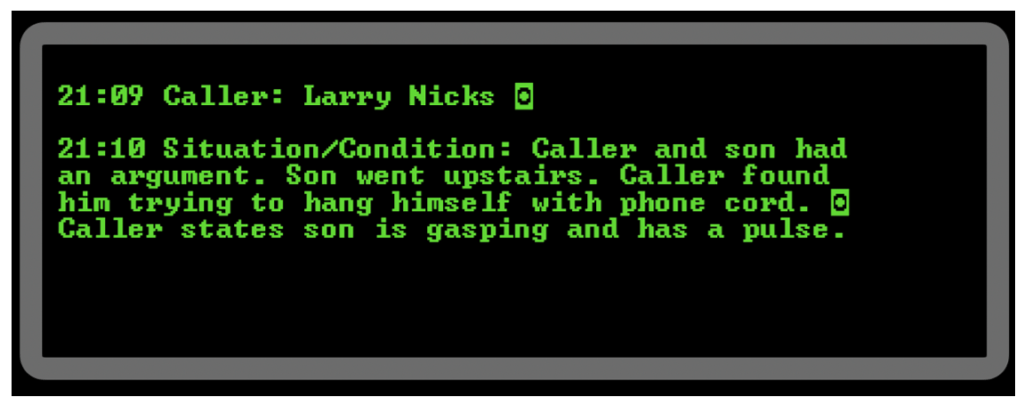
The night has been nonstop but as you arrive to the latest motor vehicle accident, the trooper waves you off signaling you aren’t needed. You give them a thumbs up, hit the in-service button on your computer-aided dispatch (CAD) system and excitedly ask your partner, “want to grab some food?” She enthusiastically smiles and enthusiastically says “hell yes!” Before you can even ask, “what’cha you want?” The CAD beeps dispatching you to a suicide attempt. You give the first few turn-by-turn directions to your partner and then read out the notes. It states:
You respond to the home and are greeted by police officers pulling up at the same time. There is a distraught older male in the front yard franticly waving. He takes you in and upstairs, the officer following first while you and your partner safely behind. As you round the corner to the room, you see a young male supine on the floor, a cord looped next to him. The father is distraught but tries to explain what happened as you begin your assessment.
Read: Friday Night Lights: Shift 1 – Balloons Under Water
He says, “Nathan and I have been fighting a lot since his mom passed. Today there was a bad argument and he stormed upstairs and slammed the door. I went up to check on him, but he did respond so I popped the door and found him hanging with a blue face. It had to have only been two-to-three minutes tops. I cut him down immediately and got him to the floor. I felt that he had a pulse and called 911.” While the father was talking you’ve managed to complete a primary assessment while your partner hooked him up to the monitor. He’s not breathing but he has a slow pulse, so you start rescue breathing.
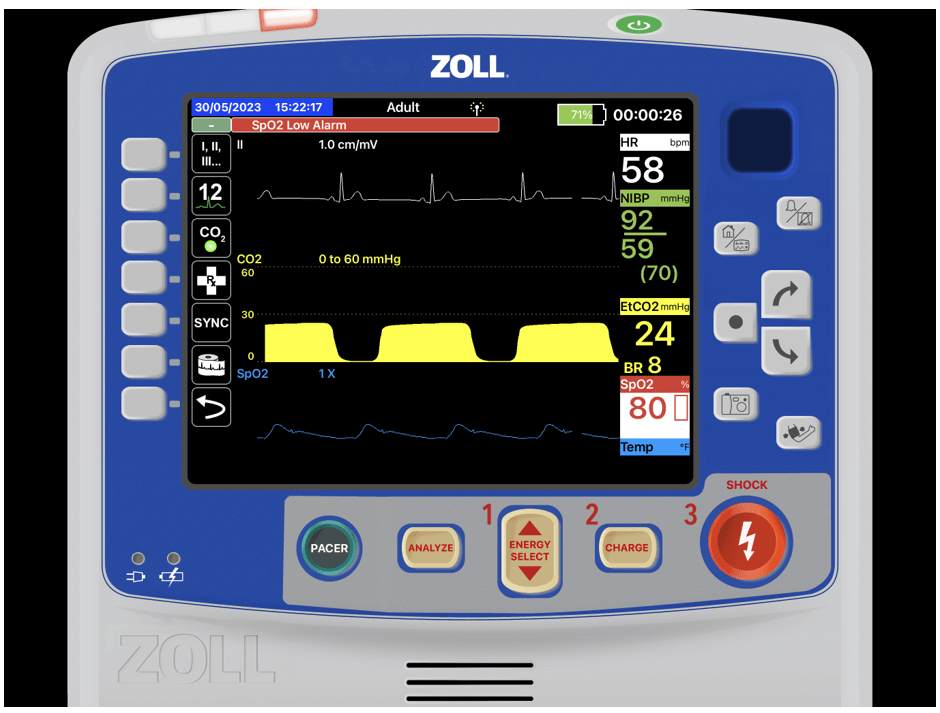
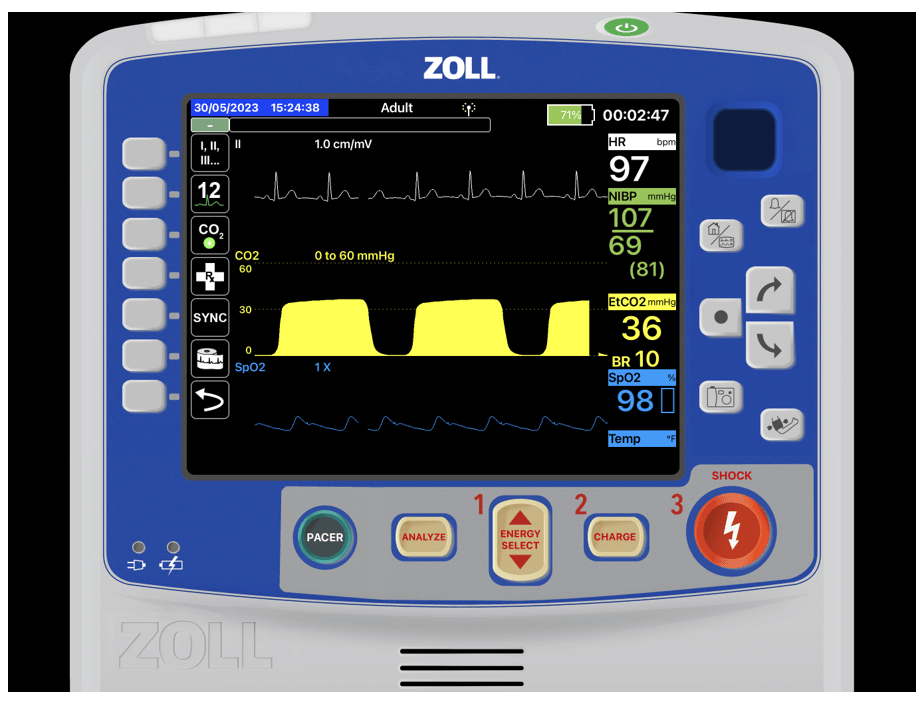
You notice he has petechiae around his neck and as you start to bag you notice his neck puffing ever so slightly. You place a collar and spinal motion restriction and then look over to the monitor.
What jumps out at you?
You ask the father if Nathan has any medical problems or any medications. He states some type of selective serotonin reuptake inhibitor and anxiolytic that he takes regularly but he has no allergies that he knows of aside from grass pollen.
You quietly get your partners attention and gesture “intubation” knowing in the back of your head that you are concerned the neck puffing could be from a fractured trachea.
Read: Friday Night Lights: Shift 2 – Leaky Hose
While your partner ventilates, you start prepping your equipment. Your bougie is your go-to since you anticipate damage to the structures. You know you can dive it in feeling for cartilaginous rings to confirm you are in the trachea even after the potential fracture point.
You also opt for a smaller than normal tube to help with success in the event the tracheal fracture has shifted. You place a 6.0mm ET tube to 20 at the lip without issue. You see bilateral chest rise with no puffing of the neck and no epigastric sounds.
Your monitor shows the following:
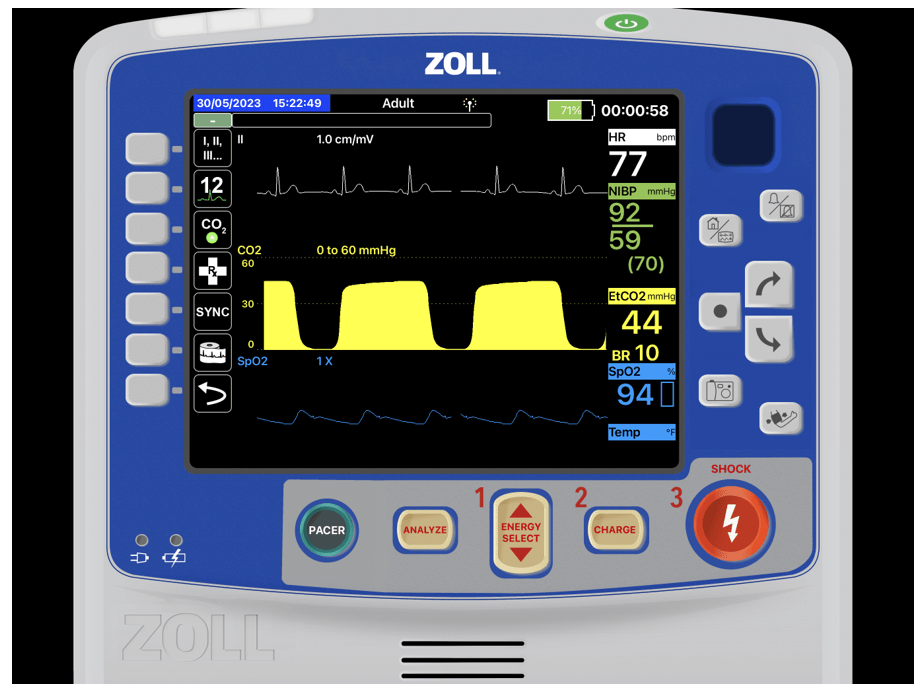
You can hear the distraught dad still repeating, “He was only up there for a minute, it could only have been a minute or two.” You ensure the officer has a chaplain on the way and ask him to keep talking to the dad gathering information and keeping him informed of your efforts.
Your partner runs out to grab the Reeves stretcher and you let the officer and dad know you plan to transport Nathan over to the university hospital. You carefully monitor capnography to ensure the tube stays in place while you carry him down the stairs, onto the cot, and load him in the unit. You reconfirm lung sounds and look over at your monitor.
Your partner hops upfront and starts to head toward the hospital, about two minutes out from the hospital you notice the following. What is this? Are you concerned?
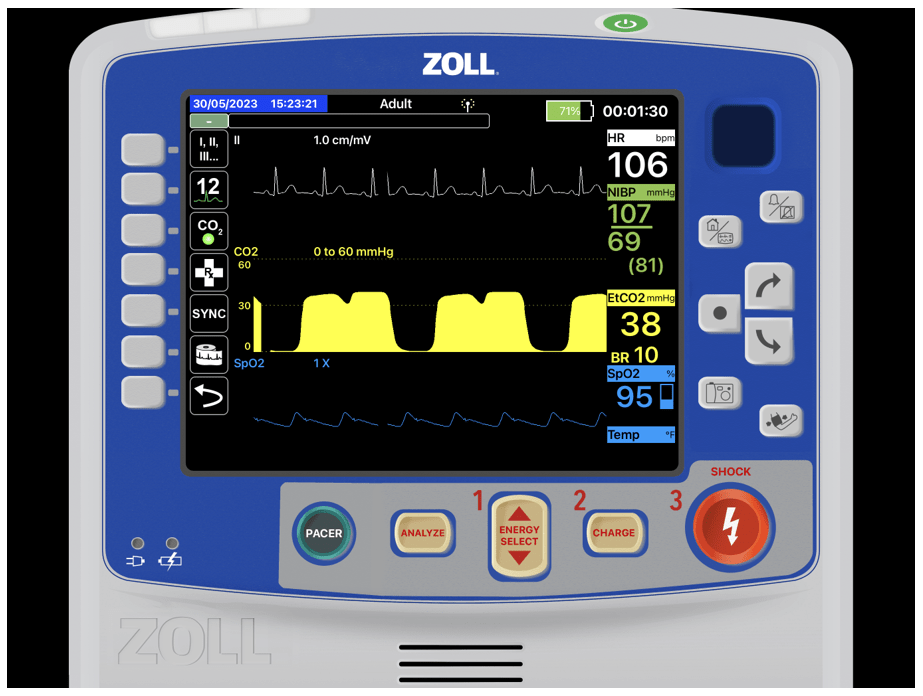
What you’re seeing is the diaphragm starting to work again, the dip in the C-D phase is called a curare cleft. This is most commonly seen when paralytics and/or sedation wear off in an intubated patient. This is indicative of the diaphragm coming back online. The patient needs to be sedated to avoid ventilatory mismatch if they are breathing out of sync with your ventilations.
Read: Friday Night Lights: Shift 3 – Above the Baseline
Also, if the diaphragm is starting to work, there is a strong possibility they’re going to start to pull out the tube. Remember the body doesn’t know the difference between the lifesaving ET tube with the 10 mL inflated cuff and a piece of steak or piece of broccoli you are choking on. Naturally, this causes a stress response and coughing/choking reflex response. You grab your ketamine and verify your dose with your cross-check app and administer it. You find the following approximately 40 seconds after the ketamine is on board.
Are you out of the water?
It isn’t uncommon for us to walk into a chaotic situation and work hard to stabilize patients and the scene. Many times, we don’t get patients back right away. We have to continue titrating drips, checking end points, and delivering therapies to continue the stabilization. This case provides a prime example of a crew coming in and stabilizing the situation and patient and then initiating transport.
While en route to the hospital, the patient starts to perk back up after the therapies that EMS provided restored oxygenation and ventilation. End-tidal capnography in this case saved the crew and the patient by shedding light on the patient status changing very early. Early enough the EMS crew was able to intervene before the patient started to wake up and bucking the tub and pulling at interventions.
Chris Kroboth has been a career paramedic/firefighter for over 17 years and in EMS for over 23. He has been in prehospital and in-hospital education for the past 18 years. His last assignment before returning to operations was as the EMS training captain in charge of continuing education programs and certification. He is also affiliate faculty with the Virginia Commonwealth University Paramedic Program. He is the U.S. clinical education manager for iSimulate and also facilitates national conference clinical challenges to include EMS World, ENA and NTI.


