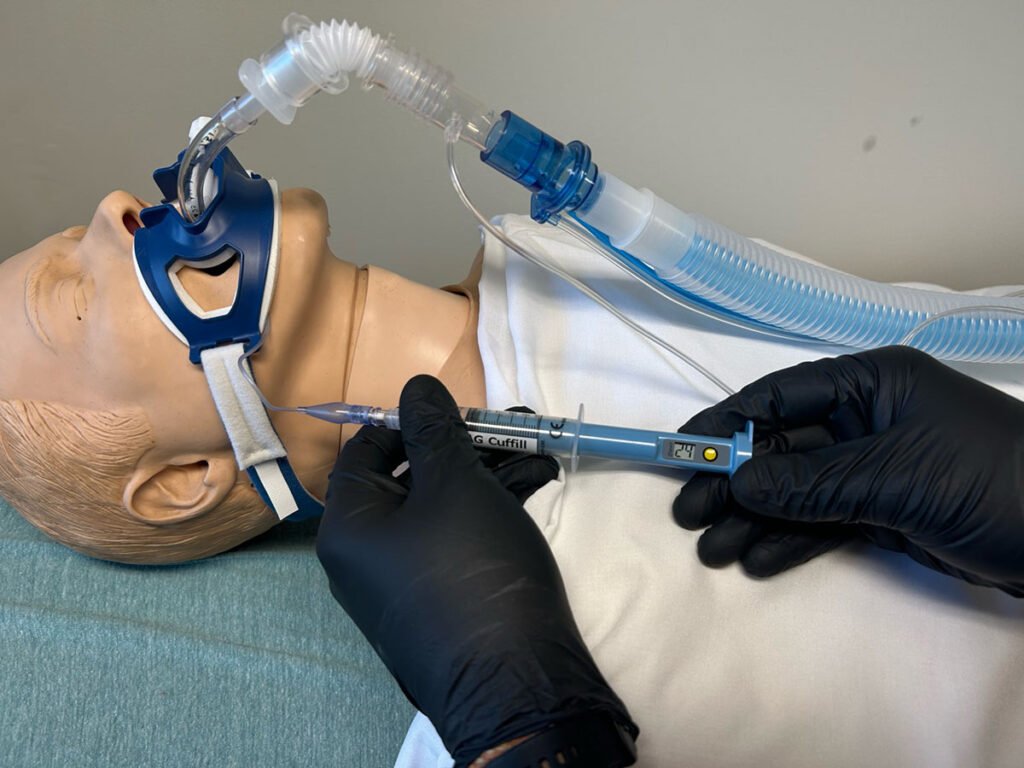
A cuff pressure mamometer in use. (Photo provided by the author.)
In 2019, our service (AirCare Critical Care Transport Team at Atrium Health Wake Forest Baptist Hospital) performed a yearlong QI review that highlighted critically high ETT cuff pressures in over 80 percent of our intubated patients regardless of who the technician was that placed the endotracheal tube.
The significance of the ETT cuff over-pressure in all our patients led us to incorporating the AF Cuffill syringe in our practice to ensure patient safety and well-being during intubation and ventilation procedures.
In 2023, we analyzed a dataset consisting of 229 sequential pressure readings recorded by AirCare Critical Care providers between January 01, 2023, and August 01, 2023. The objective of this analysis is to assess the distribution of pressure deviations from the desired range of 20 – 30 mmHg.1 The results of this review demonstrated that a quarter of our patients have endotracheal tube cuffs that are over-pressured.
The ETT cuff’s primary function is to establish an airtight seal between the tracheal tube and the tracheal wall, preventing leakage of air and secretions into the lung or surrounding tissues.
Proper inflation and pressure regulation of the cuff are essential to minimize the risk of aspiration, ventilator-associated pneumonia, and other complications related to inadequate sealing or excessive pressure on the tracheal mucosa.
Inaccurate cuff pressure can lead to tracheal stenosis, ischemia, and pressure ulcers, underlining the need for vigilant monitoring and adjustments.
Multiple studies have demonstrated the prevalence of over-pressured EET cuffs in both the prehospital and the interfacility environments.2
In the absence of the ability to accurately measure cuff pressures it has been suggest that providers utilize a cuff inflation volume of 6–7 ccs as this approach resulted in the highest likelihood of achieving the desired cuff pressure range, while cuffs inflated with 8–10 cc resulted in dangerously high CPs in all instances.3
To address this issue, healthcare institutions and professional organizations have emphasized the importance of proper ETT cuff management. Guidelines and recommendations for cuff inflation and pressure monitoring have been established to minimize the prevalence of over-pressured cuffs.
These guidelines stress the use of appropriate cuff pressure measurement devices, regular monitoring, and the involvement of trained personnel in cuff management.
AirCare providers have utilized the AG Cuffill device for ETT cuff inflation and adjustment since 2019. Our standard of care is to use the AG Cuffill device for all ETT placements and to confirm pressure and adjust as needed for all patients that we receive that already have an ETT in place. These pressure readings are recorded on the ePCR as part of our charting standards.
For the past seven months of 2023 we reviewed the charting of our providers for all instances of patient with an ETT in place or placed by the transport team. Out of the 229 readings collected, 58 instances were identified as exceeding the prescribed pressure limits, resulting in over-pressure conditions.
Conversely, a minor two instances were recorded as falling below the recommended pressure thresholds, indicating instances of under-pressure. All these deviations were attributed to endotracheal tubes that were placed by outside providers and no distinctions were made regarding the training level of those providers. These deviations emphasize the ongoing prevalence of over-inflation.
The findings underscore the significance of continuous monitoring and control measures to prevent pressure-related incidents and to ensure optimal operational conditions.
Further investigations into the causes of overpressure and under pressure events are warranted to develop targeted strategies for preventing such occurrences and enhancing system reliability.
References
- Moon, K. M., Donaworth, S., Hagele, M. S., Kim, S. S., Willer, B. L., & Tobias, J. D. (2022). Endotracheal Tube Cuff Pressures in the Operating Room of a Pediatric Hospital: A Quality Improvement Initiative. Pediatric quality & safety, 7(6), e619. https://doi.org/10.1097/pq9.0000000000000619
- Chen, R., O’Connor, L., Rebesco, M., LaBarge, K., Remotti, E., & Tennyson, J. (2021). Prehospital Intubations Are Associated with Elevated Endotracheal Tube Cuff Pressures: A Cross-Sectional Study Characterizing ETT Cuff Pressures at a Tertiary Care Emergency Department. Prehospital and Disaster Medicine, 36(3), 283-286. doi:10.1017/S1049023X21000297
- Carhart, E., Stuck, L. H., & Salzman, J. G. (2016). Achieving a Safe Endotracheal Tube Cuff Pressure in the Prehospital Setting: Is It Time to Revise the Standard Cuff Inflation Practice?. Prehospital emergency care, 20(2), 273–277. https://doi.org/10.3109/10903127.2015.1061626
Clifton Thompson, BSN, RN, CFRN, NREMT, is a critical care transport nurse in North Carolina. He is the current educator for AirCare Critical Care Transport at Atrium Health Wake Forest Baptist Hospital.



In the absence of the ability to accurately measure cuff pressures it has been suggested that providers utilize a cuff inflation volume of 6–7 ccs. Has this recommendation alone been shown to reduce the cuff pressures?
There is an inexpensive device made by a company called Vortran out of California. It is a small handheld pressure manometer that allows the provider to check and see how much pressure is in the cuff. Hospitals use devices and we should too in EMS. I think they are less than $25 and can prevent years of damage to the patient.
Both the one mentioned and the AG Cuffill device are easily acquired for the purpose of measuring cuff pressures.