Welcome back. Here is a quick recap from last time. Pediatric respiratory distress cases can leave providers with questions. What makes these cases more challenging to manage includes low frequency of events, anatomical differences from adults, differences in presentations, and disease processes, not to mention countless external, emotional factors that go into treating children.
“The why” is always essential in these cases. CPAP and BiPAP are both forms of non-invasive ventilation, and for this section, CPAP will be the common term to identify both. CPAP is a non-invasive means of delivering additional pressure into the lungs to support normal respiratory function, thus improving the efficiency of gas exchange and the patient’s overall work of breathing. Non-invasive ventilation has a long list of benefits but also has a couple of risks if applied in the wrong situations. The most significant risk is aspiration and gastric insufflation, which is most likely to occur in severely hypoxic or hypercarbic patients who cannot protect their airways or any combination of those conditions.1
Given the many risks associated with endotracheal intubation in pediatrics, including cardiac arrest,2 alternatives like CPAP that can quickly improve respiratory functions and reduce the likelihood of decompensation must be at an EMS provider’s disposal. For patients in respiratory distress who can protect their airways, CPAP can facilitate desired improvements without the risks associated with anesthesia for intubation. So much so that a recent meta-analysis study shows the rates of decompensation and subsequent need for intubation in children were lower when using CPAP vs. standard treatment.3
CPAP has history dates back to the 1940s, yet its use in pediatrics (specifically with neonates) came in the 1970s. Despite the delay, it has proven safe and effective for roughly 50 years.4 Equipment exists to deliver CPAP in the prehospital setting safely, and while widely used with adults, current data shows that EMS rarely uses CPAP in pediatric respiratory cases.5 However, multiple studies show proven benefits in pediatric cases by improving the patient’s work of breathing, reducing rates of intubation, and decreasing the rate of mortality associated with respiratory distress.6 These studies provide a solid argument for increasing the use of pediatric CPAP in the prehospital setting.
If You are Excited and Asking How It Works… Good!
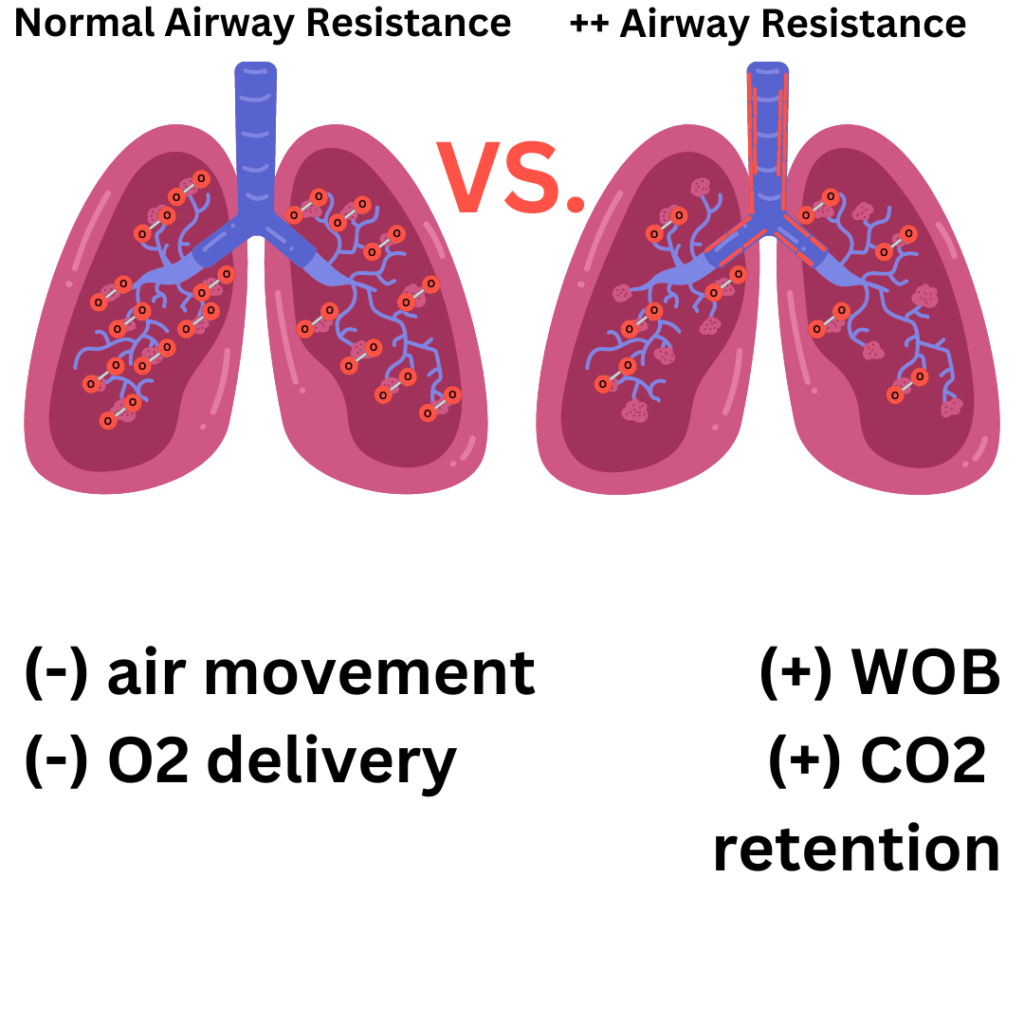
People breathe by contracting their diaphragm and the muscles in their chest to create negative pressure, thus drawing air from the atmosphere and into the lungs, and kids are no different. When things go wrong (airway constriction, mucus build, etc.), the negative pressure only goes so far, and the ability effectively ventilate decreases. A deficit begins to develop when insufficient oxygen enters the bloodstream via the lungs, and carbon dioxide cannot leave the blood. This deficit is a ventilation-to-perfusion (or V/Q) mismatch.7 CPAP helps to overcome some of the shortcomings of negative pressure ventilation when kids get sick.
Remember, a patient has to be protecting their airway and breathing effectively for CPAP to be indicated – Yes, this was said already, but it warrants repeating. Moderate to severe respiratory distress with a patent airway – CPAP is OK. Agonal respirations or apnea without a patent airway – BVM is the correct choice! Additionally, BVM should always be used for a child in cardiac arrest, especially since most childhood arrests are due to hypoxia.
In part one of this series, “Pediatric Respiratory Illness and Current Best Practices,” the following causes of pediatric respiratory distress were covered: asthma, pneumonia and bronchiolitis. Those diseases lead to inflammation and/or obstruction of gas exchange in the alveoli, and CPAP helps overcome both.
Images/Glen Keating
During inhalation, CPAP delivers pressure to supplement the negative pressure created in the chest. In cases where inflammation is present, this helps open the airways and reduces airway resistance. In cases of obstructed gas exchange at the alveoli (i.e., pneumonia), CPAP puts additional pressure on the alveoli, temporarily displacing the obstructing material and allowing gas exchange. All of this leads to more air entering the lungs and the alveoli with each breath. That air has oxygen, which will help overcome that V/Q mismatch.
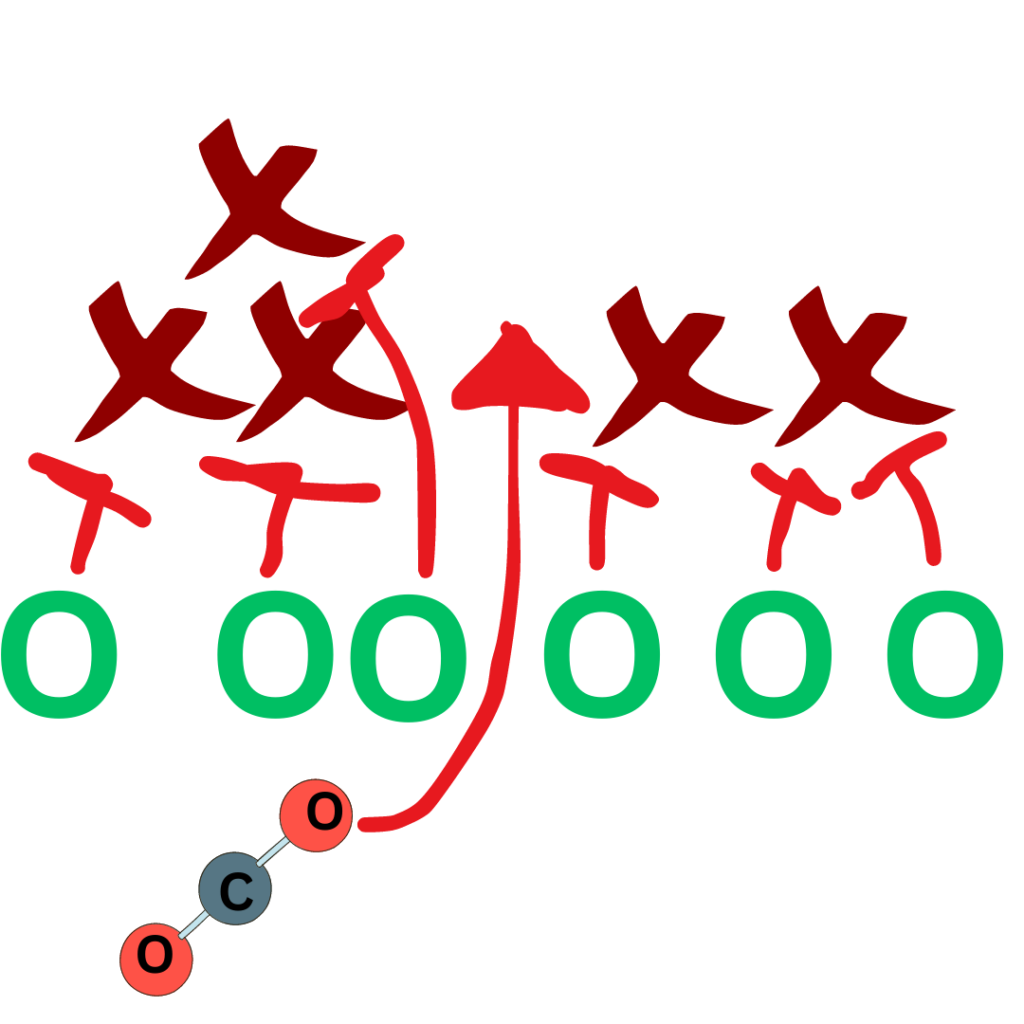
Conversely, carbon dioxide has to get out of the lungs. Intentionally forcing additional air into the lungs would not help allow for air to leave the lungs. While the pressure of CPAP is significant and supplements the negative pressure of inhalation, the natural force of exhalation is enough to overcome the CPAP pressure and allow for exhalation. Where does that CPAP pressure go during exhalation? That pressure goes up against the walls of the airways providing outward pressure and reducing airway resistance.
Some pressure from CPAP will also provide pressure in the alveoli, improving the mean airway pressure and gas exchange. On exhalation, think of CPAP as an offensive line in football, making a path against the defense (inflammation) for the ball carrier (CO2) to go through. You may also wonder about air trapping, commonly seen in COPD patients where the bronchioles and alveoli are damaged, and air can get in. However, these structures collapse on exhalation trapping the carbon dioxide inside.8 The good news is that this is not seen when CPAP is applied, as it stents open the airways even during exhalation.
Remember, any airway resistance or obstruction in the lungs in adults is terrible, but the same resistance and obstruction for kids has a multiplied negative effect. The positive pressure from CPAP helps reduce resistance and creates airway stenting and obstruction displacement, which is all exceptionally helpful, if not lifesaving, and reduces the need for intubation.6
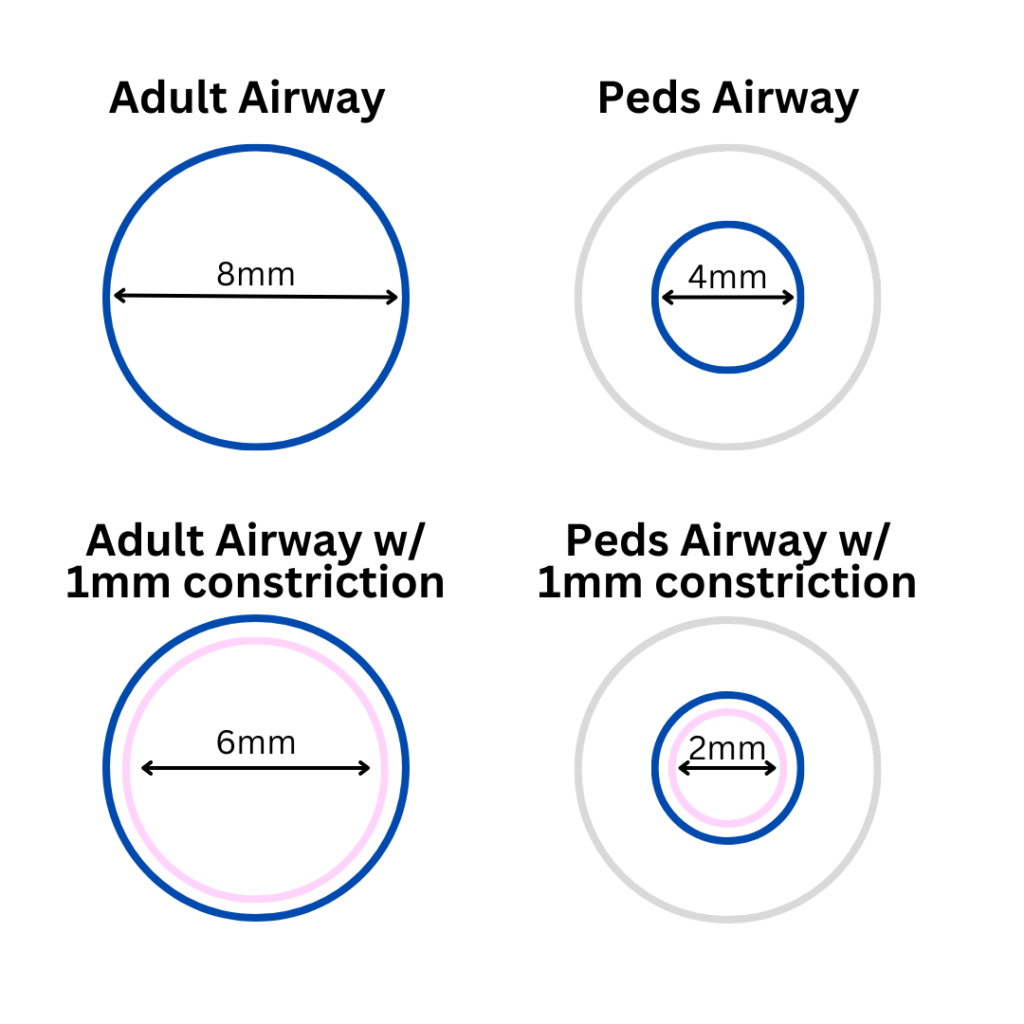
Adapted from: ADEWALE, L. (2009), Anatomy and assessment of the pediatric airway. Pediatric Anesthesia, 19: 1-8 https://doi.org/10.1111/j.1460-9592.2009.03012.x
CPAP in kids can be effective alone, or it can serve as a bridge ahead of other treatments.9 Combining other standard therapies is helpful to facilitate treatment and slow the progress of the disease process, such as asthma or pneumonia. In some patients, definitive treatment may require steroids or antibiotics, which take time to become therapeutic.
However, when CPAP is applied to these patients, there is a much lower rate of treatment failure and need for intubation.6 When considering asthma, it is important to ask about home medications such as nebulized bronchodilators. The spirit behind this and other treatments, such as inhaled corticosteroids or long-acting beta-agonists, is to treat asthma early and decrease the need for emergency intervention.10, 11
Nevertheless, when EMS is summoned despite home medications being administered, it should be assumed that standard home treatments are not enough to overcome the exacerbation, and more aggressive therapy such as CPAP is warranted.
So, what is needed to implement pediatric CPAP into any EMS system?

Some providers may not have CPAP for adults or pediatrics in their system for a variety of reasons, but if your agency have the means and want to implement or improve pediatric CPAP in your system, here are some ideas for how to make it a reality:
- First, know your population. Query your cases, look for when it could have been helpful, and review how care was provided to these patients. Objective data on past cases can help get an idea for the future. Now is also an excellent time to browse the equipment cost, the ongoing delivery cost, and the potential for cost recovery through billing reimbursement.
- Build a protocol. Work closely with your medical director and your local children’s hospital for guidance. This collaboration is also useful so that receiving facilities know what care is being provided in the field and what to expect from EMS teams in the future.
- Select your equipment. Various cost-effective prehospital CPAP systems are on the market today, and some agencies may elect to deliver CPAP via a transport ventilator. Sometimes adapting adult equipment to work for kids means an extra fitting, but sometimes it is much more. Research the options that are available and work with suppliers for the best solution for your system. Remember to leverage relationships with the children’s hospital for additional support.
- Provide training and simulations. Consider using external training and (not to sound like a broken record) reach out to your local children’s hospital for further assistance and guidance. The training and simulation period is a great time to discuss with crews how the equipment should be packaged and made available for application. Some may include it with a pediatric bag; others may elect to put it in with other CPAP equipment – whatever fits the system.
- Establish quality metrics. How can you evaluate your pediatric CPAP program if you do not measure it? This starts with simple metrics like how often it is being deployed and when, and asking, “When should it have been deployed?” Keep digging to ensure the right kind of vital signs are being assessed (including ETCO2) and documented and that other interventions are being administered. Work closely with your medical directors and children’s hospital to ensure these are all consistent with best practices or develop a plan to improve. The quality assurance and improvement process is vital to validate the training and the delivery of pediatric CPAP in a meaningful, safe way.
- Plan a rollout. When planning, look at the need for pediatric CPAP, department size, provider familiarity, and any other factor that may have an impact. Some elect to put it on every vehicle immediately; others may try a pilot project in a targeted geographical area. Completing “small tests of change” is a common technique in healthcare quality improvement, but what those small tests look like is not a universal standard. Seek the input of stakeholders (providers, administration, medical direction, local hospital) to discern the best way to go live with this in your system.
- Get follow-up reports. When crews encounter pediatric respiratory distress patients, debrief the cases, have honest conversations about how it went and where improvements can be made, and celebrate wins. Pediatric respiratory distress encounters can be scary, so make sure to talk it out and show appreciation to crews and providers who make a positive impact despite the challenges of pediatric patients.

Conclusion
CPAP is a non-invasive means of assisting ventilation that is safe to administer for pediatrics who maintain their airway. CPAP is very effective at reducing rates of treatment failure and intubation. During inhalation, it works by helping overcome resistance and also displacing obstructions in the alveoli, such as mucus. During exhalation, it continues to stent airways open, which facilitates CO2 expulsion and also further improves oxygen diffusion in the alveoli.
Implementation includes many considerations, including what sort of need exists, what equipment should be used, what the protocol and training should look like, and how to do adequate quality assurance and improvement after implementation. A key theme is to utilize your agency’s medical director and the resources of your local children’s hospital.
While many large lifts are associated with implementing pediatric CPAP, it is a worthwhile endeavor for our pediatric patients and hopefully the answer to many questions that arise during these cases. The ability to safely do more can be a life-saving relief to patients, providers and families alike.
References
1: Josiah C. Daily & Henry E. Wang (2011) Non-invasive Positive Pressure Ventilation: Resource Document for the National Association of EMS Physicians Position Statement, Prehospital Emergency Care, 15:3, 432-438, DOI: 10.3109/10903127.2011.569851
2: Fiadjoe JE, et al. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med. 2016 Jan;4(1):37-48. doi: 10.1016/S2213-2600(15)00508-1. Epub 2015 Dec 17. PMID: 26705976.
3: Boghi, Daniele MD; et al. Non-invasive Ventilation for Acute Respiratory Failure in Pediatric Patients: A Systematic Review and Meta-Analysis. Pediatric Critical Care Medicine 24(2):p 123-132, February 2023. | DOI: 10.1097/PCC.0000000000003109
4: Pierson, David J; History and Epidemiology of Non-invasive Ventilation in the Acute-Care Setting. Respiratory Care 2009 Jan; 54 (1): 40-52; https://rc.rcjournal.com/content/54/1/40
5: Erin R. Hanlin, et al. Epidemiology of out-of-hospital pediatric airway management in the 2019 national emergency medical services information system data set, Resuscitation, Volume 173, 2022, Pages 124-133, ISSN 0300-9572, https://doi.org/10.1016/j.resuscitation.2022.01.008.
6: Wang Zhili, et al. Non-Invasive Ventilation Strategies in Children With Acute Lower Respiratory Infection: A Systematic Review and Bayesian Network Meta-Analysis, Frontiers in Pediatrics Volume 9, 2021, ISSN 2296-2360, https://doi.org/10.3389/fped.2021.749975
7: Raouf S. Amin, Chapter 14 – Chronic Respiratory Failure, Editor(s): Victor Chernick, Thomas F. Boat, Robert W. Wilmott, Andrew Bush, Kendig’s Disorders of the Respiratory Tract in Children (Seventh Edition), W.B. Saunders, 2006, Pages 243-258, ISBN 9780721636955, https://doi.org/10.1016/B978-0-7216-3695-5.50018-3.
8: Kim Y, et al. Air Trapping and the Risk of COPD Exacerbation: Analysis From Prospective KOCOSS Cohort. Front Med (Lausanne). 2022 Mar 11;9:835069. doi: 10.3389/fmed.2022.835069. PMID: 35372402; PMCID: PMC8965692.
9: Chad D. Viscusi, Garrett S. Pacheco, Pediatric Emergency Non-invasive Ventilation, Emergency Medicine Clinics of North America, Volume 36, Issue 2, 2018, Pages 387-400, ISSN 0733-8627, ISBN 9780323583503, https://doi.org/10.1016/j.emc.2017.12.007.
10: Zimo DA, Gaspar M, Akhter J. The efficacy and safety of home nebulizer therapy for children with asthma. Am J Dis Child. 1989 Feb;143(2):208-11. doi: 10.1001/archpedi.1989.02150140102029. PMID: 2563627.
11: Cloutier MM, Teach SJ, Lemanske RF, et al. The 2020 Focused Updates to the NIH Asthma Management Guidelines: Key Points for Pediatricians. Pediatrics. 2021; 147(6):e2021050286
Glen Keating is an airway enthusiast from Columbus, Ohio. Glen is paramedic in charge of quality improvement for a suburban EMS system north of Columbus and spent 11 years as a respiratory therapist at a Level-One trauma center in Columbus. He holds a Bachelor of Science degree in emergency medical care from Eastern Kentucky University and is an Ohio EMS Instructor with a special focus on airway and ventilation management. He is the owner of PreHospital Elements, LLC., an EMS education and quality improvement firm based in Ohio.


