On the go? Listen to the article in the player below!
You arrive on scene and find a 68-year-old man is lying on the couch with difficulty breathing. He’s obese and obtunded, with severe respiratory distress.
His wife tells you he has a history of congestive heart failure. He appears pale and diaphoretic, with snoring, slow, shallow breaths and his initial oxygen saturation is 72%. What are the most important first steps in managing his airway and breathing?
PATIENT POSITIONING
The most crucial factor in airway management is patient positioning. Improper positioning can, and frequently does, inhibit effective ventilation and oxygenation.
It’s commonly taught that patients must be supine to enable airway management. This teaching is flawed, as supine is the most dangerous position for a patient with a compromised airway. The most detrimental position for a patient, from an airway perspective, is flat on their back. Supine is best described as the “COFFIN position,” or “Cannot Oxygenate Face Flat In Neutral position.”
Why is supine such a compromising position? The primary reason is the tongue. If a healthy person lies on their back, their intrinsic reflexes maintain upper airway tone, which keeps the tongue from occluding the airway. But, when a patient with airway compromise is on their back, the tongue falls to the posterior pharynx. Additionally, the soft tissues of the upper airway relax and contribute to compression of the pharynx narrowing the airway.1 This can sometimes be managed with basic airway maneuvers, but can often be addressed simply by optimizing positioning.
Supine positioning also significantly reduces lung capacity due to compression of the diaphragm and chest by soft tissue. Additionally, almost all airway interventions are more difficult in the supine position. This is especially true for bag-valve mask (BVM) ventilation, as upper airway collapse makes ventilation significantly more challenging. Mask seal is also more challenging as the soft tissue of the face falls posteriorly.
Overall, airway management is improved in the upright position. The initial response to a patient with airway compromise and a decreased level of consciousness should be “OOPS,” or, “Oxygen On, Pull the Mandible Forward, Sit the Patient Up.”2 Oxygen should be applied via nasal cannula at 15 Lpm or higher.
Traditionally, it’s taught that the nasal cannula can only be used up to 6 Lpm but it’s actually capable of effectively delivering much higher flow rates.3
Higher flow rates are necessary in cases of severe distress as patients regularly generate negative inspiratory flow rates in their airway of more than 30 Lpm. Oxygen delivery must be titrated to match the patient’s demand.
Keep in mind that nasal cannulas capable of end-tidal carbon dioxide (EtCO2) monitoring typically can’t deliver flow rates higher than 6 Lpm. This is because the oxygen is delivered via small holes above the nasal prongs and not from the prongs themselves.
The nose is the ideal route to provide oxygen … applying ‘Os up the nose’ is the best initial response to hypoxia.
The nose is the ideal route to provide oxygen. The nasopharynx acts as a reservoir that can fill with a high concentration of oxygen that the patient can utilize on inspiration. Applying “Os up the nose” is the best initial response to hypoxia.
Sitting the patient up takes them out of the compromising supine position and helps to open the upper airway. Once upright, applying a significant jaw thrust will further open the airway by pulling the tongue and soft tissues forward, away from the posterior pharynx. This will allow nasal oxygen to passively begin to oxygenate the patient.
Additionally, it’s been demonstrated that the head-tilt-chin lift technique that’s commonly taught does not open the airway. The jaw thrust is the most effective basic airway maneuver.
OOPS as an initial response to airway compromise will rapidly address many likely causes of respiratory failure and start to improve the patient’s condition.

The initial response to a patient with airway compromise and a decreased level of consciousness is not to keep them supine, but to follow OOPS: Oxygen On, Pull the Mandible Forward, Sit the Patient Up.
CASE (CONTINUED)
You recognize that your patient has immediate airway compromise. Due to his size and supine position on the couch, the quickest thing you can do is elevate his head, which you do by placing towels underneath. This somewhat improves the snoring being caused by his tongue.
Pillows are then placed underneath his back and head to maintain that position. Once upright, you apply a nasal cannula at 15 Lpm and perform a jaw thrust by pulling the mandible forward maximally. His snoring stops, and you begin to see some improvement in the pulse oximetry. However, you recognize that he needs further intervention.
OXYGENATION & VENTILATION
After applying the OOPS principles, the next step is to decide whether the patient has a ventilation problem as well as an oxygenation problem. Many patients will have significant improvement in oxygenation with only the nasal cannula and may not need further intervention. However, we have many prehospital resources to address patients who require more assistance.
The most frequently taught intervention for the hypoxemic patient is the non-rebreather (NRB). However, the NRB is a flawed device for several reasons. It’s a myth that an NRB can provide > 90% fraction of inspired oxygen (FiO2). In reality, NRBs typically used in the emergency setting can only deliver about 60–70% FiO2.4
The primary reason for this is that most NRBs don’t come with two exhalation valves; they only have one. This means that room air is entrained into the mask every time the patient inhales.
Another factor is that the NRB mask is rarely sealed properly to the patient’s face. This is another way that room air can leak into the mask and lower the FiO2.
You may have seen a patient in respiratory distress pull an NRB off their face. We typically say that “they wouldn’t tolerate” the NRB. But why do patients do that? Don’t they know the NRB helps? The reason is that, at 15 Lpm, an NRB may not provide enough flow to match the patient’s minute volume.5
A person with normal respiratory status has a minute volume of about 6–7 Lpm. But a patient in respiratory distress will be breathing faster and deeper, and could easily have a minute volume > 15 Lpm. Additionally, the liter flow of oxygen must match the patient’s high negative inspiratory flow rate in the airway.
If the NRB is truly fitted to the patient’s face and isn’t matching their demand, they will feel air hungry, and this leads them to pull the mask off. However, combining an NRB with a nasal cannula provides higher flow rates that may be able to match your patient’s demand.
CASE (CONTINUED)
With OOPS being performed, you consider the best next steps to improve the patient’s respiratory status. Your partner quickly applies an NRB at 15 Lpm. However, as an NRB doesn’t help with work of breathing, the patient still appears in significant distress—and his oxygen saturation has only improved to 81%.
POSITIVE PRESSURE
Some patients will need more support, as a nasal cannula and NRB don’t improve respiratory function, they only increase the oxygen concentration that the patient is breathing. Additionally, patients with lung disease and poor respiratory effort have pulmonary shunt. This is caused by atelectasis or lung infiltrates, such as fluid or infection that interfere with the function of alveoli in a particular area of the lung.
These situations require an increase in mean airway pressure, typically by using continuous positive airway pressure (CPAP) or assisting with a BVM. Delivering positive end expiratory pressure (PEEP) and positive pressure ventilation can re-inflate, alveoli that have collapsed or are filled with fluid.
CPAP or a BVM should always be used in combination with a nasal cannula. Adding a nasal cannula increases FiO2 and doesn’t typically interfere with mask seal.6 Patients who are candidates for CPAP have adequate respiratory effort but are still in significant distress. It isn’t as effective in patients who are fatigued or have diminishing respiratory effort. Patients should also be able to follow commands and be open to coaching for CPAP to be utilized.
CPAP is simply a method of delivering PEEP. Increasing PEEP raises the mean airway pressure, and this will improve oxygenation and help recruit alveoli. It can typically be titrated as high as 15 cmH2O. It’s recommended to start at 5 cmH2O for all patients and increase pressure as needed. This practice improves patient tolerance of the procedure, which is one of the most crucial factors in ensuring CPAP is successful.
Be sure to brief the patient before applying the mask, so they know what to expect. Apply the mask slowly and coach them through each step as they take their first assisted breaths. In some cases, it may be appropriate to use sedative agents such as benzodiazepines to help improve CPAP tolerance. However, it’s important to exercise extreme caution when using sedatives in patients with severe respiratory distress. Even small doses of benzodiazepines can decrease respiratory drive and cause respiratory failure. Ketamine may be a better option as it’s less likely to decrease respiratory drive.
Patients who have insufficient respiratory effort or are otherwise not CPAP candidates require BVM ventilation. This skill is notoriously performed poorly. The problem is that it’s often taught as an easy, “basic” procedure that doesn’t require practice. This mindset causes providers to downplay its importance during resuscitation of a critically ill patient and, in many cases, the most junior member of the crew is assigned to the BVM without supervision.
Ventilation is often the most important intervention being performed, & doing it correctly should be a priority.
The reality is that ventilation is often the most important intervention being performed, and doing it correctly should be a priority. Without conscious awareness, the tendency is for providers to ventilate too fast and with excessive volume.
Proper BVM technique is composed of three main principles: 1) consistent mask seal; 2) proper tidal volume; and, 3) controlled rate. Mask seal is best optimized by using a two-person technique.
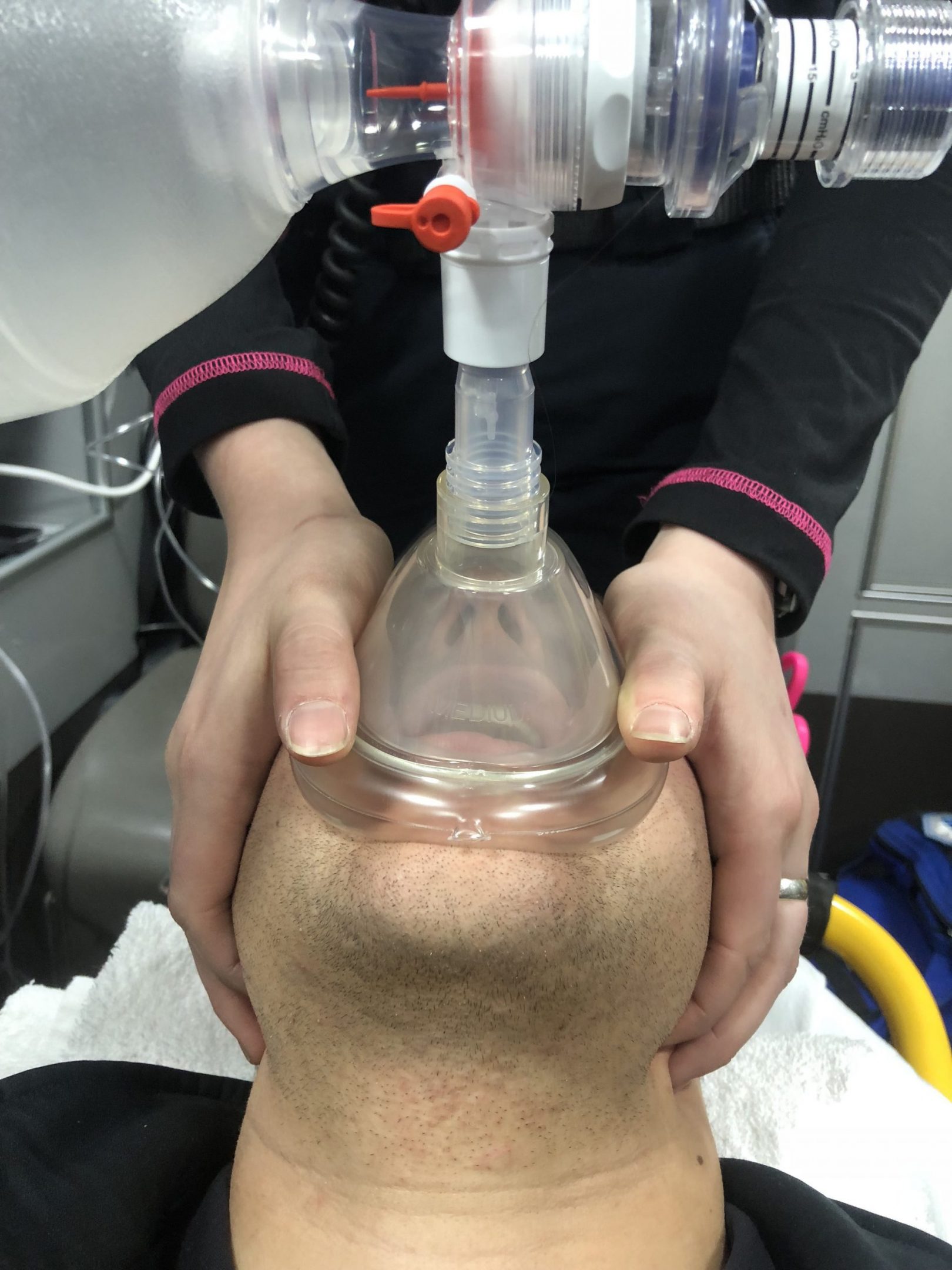
The ideal way to ensure a proper mask seal using a two-person approach is for one provider to place the pads of the hand and the thumbs on the mask, while the second provider uses their index and other fingers to pull the jaw forward maximally.
The ideal way to obtain an excellent seal is by placing the pads of the hands and the thumbs on the mask and using the index and other fingers to pull the jaw forward maximally. This technique provides sufficient pressure to seal the mask and delivers a strong jaw thrust to maintain airway patency. This method is recommended over the traditional “C-E” when using a two-person approach.
When a one-person technique is necessary, “C-E” is the best option for mask seal. The biggest detriment to the “C-E” technique is that the provider only has their pinky and ring fingers available to perform a jaw thrust. These fingers are weaker and can’t easily displace the jaw to open the airway.
After the mask seal, squeezing the bag properly is the other critical component of BVM use. A standard adult BVM has a volume of about 1,000–1,200 mL. Most adult patients only need around 400-500 mL of volume delivered in each breath. This means that providers should use one hand and attempt to only squeeze about half or less of the volume of the bag in each breath.Using lower volumes and squeezing slowly also reduces the chance of filling the stomach with air and causing vomiting. One way to ensure more appropriate tidal volumes is to use a pediatric BVM for adult patients. They generally provide a volume of 400–600 mL, which is perfect for adults.7
Additionally, the person squeezing the bag must consciously limit the ventilatory rate to avoid over-ventilation. It’s common to see providers over-ventilating as they aren’t focused on the task and are under an adrenaline surge.8 Ventilatory rate should typically be somewhere between 10–20 bpm, depending on patient condition. EtCO2 titrated to 35–45 mmHg can help guide ventilatory rate.
In addition to good technique, there are a few ways the BVM should be optimized to ensure the patient gets the best quality ventilation. The first is that all BVMs should have PEEP valves installed. Without a PEEP valve, a BVM doesn’t maintain airway pressure even if the mask seal isn’t broken. This means that any improvement in lung function is lost between breaths, as no pressure is accumulated in the lungs.
A PEEP valve ensures that when the mask seal is maintained, the airway pressure remains at a minimum level between breaths to help keep the alveoli inflated. PEEP valves can typically be set anywhere from 5–20 cmH2O. As a rule, the worse a patient’s oxygenation is, the higher the PEEP valve should be set. For example, patients with severe pulmonary edema often require high PEEP levels to displace fluid and recruit alveoli.
The other way a BVM should be optimized is by using capnography. An inline EtCO2 adapter can be placed between the bag-valve and the mask. If the mask seal is maintained, an EtCO2 waveform will be generated and provide valuable feedback about the quality of ventilation. If there’s no EtCO2 waveform, you know that ventilation isn’t occurring and a change needs to be made.
CASE (CONTINUED)
Recognizing that your patient is obtunded and has poor respiratory effort, you decide to initiate BVM ventilation. You ensure that your BVM has EtCO2 attached and a PEEP valve set to 10 cmH2O.
With the patient sitting upright and the nasal cannula still in place, you perform a two-handed mask seal. Your partner begins squeezing the bag and initiates slow, controlled breaths in sync with the patient’s own.
An EtCO2 waveform appears, so you know ventilation is occurring. You see improved chest rise, skin color, and work of breathing. The patient’s oxygen saturation improves to 95%. At this point, you’re ready to extricate the patient to the ambulance and begin transport.
SUPRAGLOTTIC DEVICES
One of the most important recent developments in airway management is modern supraglottic devices. They’ve evolved quickly, and today, they are more effective and easier to insert than ever before—so much so that many surgical procedures under general anesthesia are being performed with laryngeal mask devices in lieu of endotracheal intubation.
The most revolutionary of these devices is the laryngeal mask style airways. The third and fourth generation devices of this type have improved mask design, and are made to function under patient movement and with secretions in the airway. Additionally, they’re easier to insert than older laryngeal mask devices or other supraglottic airways.
These modern airway adjuncts have changed the way we approach BVM ventilation. We know that ventilating with a mask is often difficult and can cause gastric distention. In patients who can tolerate it and don’t have an intact gag reflex, a laryngeal mask airway should be utilized when BVM ventilation is necessary. Inserting the device is quick and easy, and it allows more definitive and effective ventilation and airway control. It eliminates the need for a handheld mask seal while significantly lowering the risk of gastric insufflation and vomiting. In fact, upper airway collapse actually improves laryngeal mask functionality as the airway tissues collapse into the bowl and improve the mask seal. These principles are also true in cardiac arrest. If a BVM is going to be used, placing a laryngeal mask is beneficial.
CASE (CONTINUED)
Upon moving your patient to the stretcher, you note that his breathing is slowing and his mental status is decreasing. You keep him sitting upright, elevate his head and continue BVM ventilation. Your partner prepares a laryngeal mask and you insert it rapidly, confirming placement with waveform EtCO2 while beginning bag valve ventilation.
CONCLUSION
Basic airway management has evolved significantly in recent years. Techniques and devices are being developed and changing constantly. Modern concepts, such as OOPS, O’s up the nose, upright positioning, and laryngeal masks, improve our ability to oxygenate critically ill patients and are helpful to EMS providers of all levels.
REFERENCES
1. Fouke JM, Strohl KP. Effect of position and lung volume on upper airway geometry. J Appl Physiol. 1987;63(1):375–380.
2. Levitan R. (Jan 11, 2017.) Should emergency physicians abandon face-mask ventilation? ACEP Now. Retrieved Feb. 17, 2018, from www.acepnow.com/article/ emergency-physicians-abandon-face-mask-ventilation.
3. Levitan R. (2013). The neglected orifice. Emergency Physicians Monthly. Retrieved Feb. 17, 2018 from www.epmonthly.com/article/the-neglected-orifice/.
4. Weingart S, Levitan, R. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59(3):165–175
5. Brindley PG, Beed M, Law JA, et al. Airway management outside the operating room: How to better prepare. Can J Anaesth. 2017;64(5):530–539
6. Brown DJ, Carroll SM, April MD. Face mask leak with nasal cannula during noninvasive positive pressure ventilation: A randomized crossover trial. Am J Emerg Med. Dec. 2, 2017. [Epub ahead of print.]
7. Siegler J, Kroll M, Wojcik S, et al. Can EMS providers provide appropriate tidal volumes in a simulated adult-sized patient with a pediatric-sized bag-valve-mask? Prehosp Emerg Care. 2017;21(1):74–78.
8. Khoury A, Sall FS, De Luca A, et al. Evaluation of bag-valve-mask ventilation in manikin studies: What are the current limitations? Biomed Res Int. 2016;2016:4521767.
Andrew Merelman, BS, NRP, FP-C, is a critical care paramedic working in New Hampshire. His primary interests are airway management, point-of-care ultrasound, and resuscitation. He will be starting medical school in 2018. Contact him at [email protected] or via Twitter @amerelman.
Richard Levitan, MD, FACEP, is an emergency physician with an interest in airway management. He teaches a monthly cadaver lab focusing on airway procedures and lectures worldwide. He has published many articles on airway and oxygenation techniques.




great stuff
Is there a way to be able to print this article or e-mail it? If we have established that the volume should only be 400-600 mL, why haven’t the BVM makers changed the size of the BVM on adults?