You arrive at the bedside of a ventilated patient needing a 50-minute helicopter transport to a higher level of care. The transport ventilator and circuit have been pre-use checked for integrity. Enroute, you were able to re-familiarize yourself with the ventilator you haven’t used in over a month. You and your partner reviewed oxygen consumption for this transport and have determined you have 150 minutes of available oxygen, even if the patient needed an FiO2 of 1.0. The RN caring for the patient states the current ventilator settings are pressure-regulated volume control (PRVC), respiratory rate of 16, tidal volume 450 mL, PEEP of 5 CWP, and FiO2 of 0.6. Your partner discretely whispers in your ear: “We don’t have a PRVC.” This is not an un-common scenario. Understanding acronyms and how they describe modes is essential when managing a mechanically ventilated patient.
First and foremost is understanding how the PRVC mode interacts with the patient. The first consideration is the initial ventilator settings. Remember, the ventilator is a flow generator set to target either volume or pressure. In this case you recognize a tidal volume of 450 mL has been set. To determine the actual mode, identify the patient’s ability to draw a spontaneous breath. If the patient triggers a breath and is consistently given the 450 mL tidal volume, you can surmise that ventilator is in assist control (AC) mode. If you see SIMV or IMV on a ventilator and the patient can take spontaneous breaths in-between the set breath rate, then it is most likely delivering synchronized intermittent mandatory ventilation (SIMV). In SIMV mode, a pressure support (PS) should be added to overcome any airway resistance (Raw) contributed by the endo-tracheal tube (ETT) or the patient’s airways.
Previous: Demystifying Ventilator Modes: It’s Not That Complicated!
PRVC is considered an advanced dual-control or adaptive mode. This is because the ventilator uses both volume and pressure to automatically adjust to the patient’s ventilatory needs breath by breath.1 This helps to guarantee a set tidal volume and uses a decelerating flow pattern which may help in patient to ventilator synchrony. The mechanical ventilator delivers the lowest pressure and appropriate flow needed to meet the set tidal volume target for each delivered breath.1, 2 PRVC provides the advantages of a pressure delivered breath which entails the decelerating flow available to the patient and assuring a set tidal volume. It is important to note that PRVC can be used with assist control (AC) or synchronized intermittent mandatory ventilation (SIMV), therefore determining what mode they are currently on is important.
Back to our original question: “What do I do if I don’t have PRVC on my ventilator?” There are a few options that may require some further discussion with your partner, medical control, respiratory therapist, and nurse. The first step is to confirm that the current setting are providing optimal oxygenation and ventilation, using a recent arterial blood gas (ABG).
Next, based on the current ventilator settings, you know that the patient is receiving a target tidal volume. At this point, it is paramount to understand your ventilator’s capabilities. On most transport ventilators that target a volume, flow to the patient is fixed based on the volume delivered and the inspiratory time set by the respiratory therapist. This may or may not be an issue. If the patient is “air hungry,” a pressure target may be more helpful. In a pressure targeted breath, the flow available to the patient is usually limited to the machines flow capability with a decelerating flow waveform. If the patient requires greater flow than a target tidal volume setting can deliver, then switching to a pressure target may better meet the patient’s ventilatory demand.
Remember that in PRVC, the patient gets the benefit of a guaranteed volume using a pressure delivered breath. When managing a patient ventilated with volume targeted breaths, it’s important to monitor the peak inspiratory pressure (PIP), which fluctuates with changes in lung compliance (Cst) and airway resistance (Raw). Conversely, when managing a patient receiving pressure targeted breaths, monitor the exhaled tidal volume (Vte) which will fluctuate with changes in lung compliance (Cst) and airway resistance (Raw). In the majority of cases you will encounter, patients will do fine using volume targeted breaths.
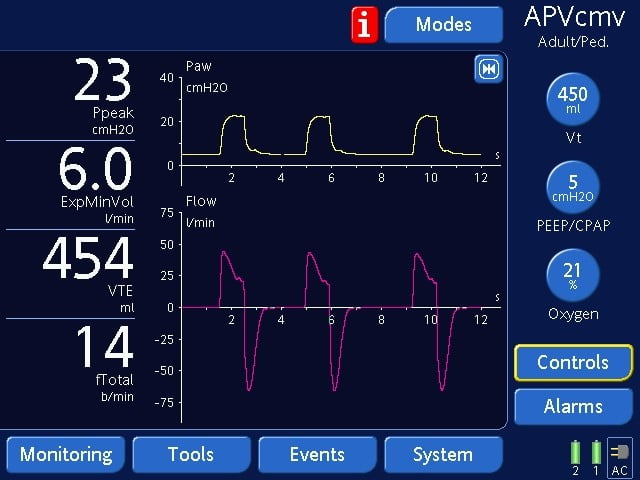
A Volume Targeted Breath
Above screen shows a Volume target (Vt) of 450 ml on the right column. The most important monitored value that needs to be observed is the peak inspiratory pressure (PIP or Ppeak) on the left column.
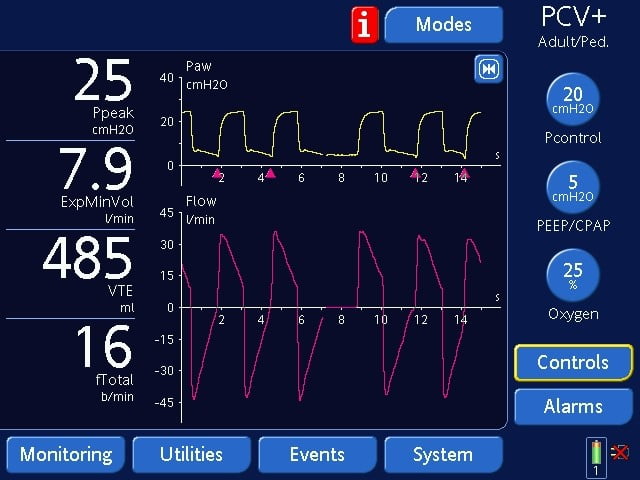
A Pressure Targeted Breath
Above screen shows a Pressure target (Pcontrol) of 20 cmH2O on the right column. The most important monitored value that needs to be observed is the exhaled tidal volume (Vte) on the left column.
In the above scenario, the patient was placed on a volume targeted breath at 450 mL and the team decided to use assist control mode. The patient had no lung disease and the ABG was within normal limits. The main concerns when choosing a mode should be ensuring patient safety and comfort (referred to as patient synchrony with the ventilator) and implementing a lung protective strategy that meets the desired oxygenation and ventilation goals.3 More articles will follow discussing more sophisticated modes and adjustments that can make a big difference in patient safety and comfort.
References
1. Cairo, J.M. (Ed.). (2020). Chapter 5: Selecting the ventilator and the mode. InPilbeam’s mechanical ventilation: Physiological and clinical applications(7th ed., pp. 58-79). St. Louis: Elsevier.
2. Holt, G.A., Habib, S.A., Shelledy, D.C. (2020). Chapter 3: Principles of mechanical ventilation. In D.C. Shelledy, J.I. Peters (Eds.),Mechanical ventilation(3rd ed., pp. 95-154). Burlington, MA: Jones & Bartlett Learning.
3. Mejia, A. (Ed.). (2023). Chapter 7: Ventilation. In Critical Care Transport (3rd ed., pp.240-241). Burlington, MA: Jones & Bartlett Learning.
Michael Schauf, RRT-NPS, has been a registered respiratory therapist at Albany Medical Center Hospital in New York since 1994. He covers all in-patient units, ICUs, the adult and pediatric Emergency Departments and is a member of the neonatal/pediatric transport team at this Level I Trauma and Level 3 NICU Center. Michael is the founder of Vent-Pro Training, teaching medics and nurses around the world how to manage mechanically ventilated patients during ground, rotor, and fixed-wing transports. He has been a flight respiratory therapist since 1998, currently working for AirMed and as a clinical education specialist for AMR. Michael authored the respiratory chapter of, “Critical Care Transport, 2nd edition,” published by Jones & Bartlett and is an adjunct instructor in the Respiratory Care Program at Hudson Valley Community College.


