A common question when managing a mechanically ventilated patient is, “which mode best fits this patient’s respiratory needs?” How do you best determine an initial ventilator mode? Is the patient on the most appropriate mode at the present time? How many modes are available on a specific ventilator?
Choice of modes should depend on clinical goals, coupled with an understanding of ventilator breath design features.1 Contrary to popular belief, there is no globally uniform definition of ventilator modes. Many modes, in fact are ventilator-brand specific. One definition that makes sense to this author is: A ventilator mode can be defined as a set of operating characteristics that control how the ventilator functions. An operation mode determines the way a ventilator is triggered into inspiration and cycled into exhalation, what variables are limited during inspiration, and whether or not the mode allows only mandatory breaths, spontaneous breaths, or both.2
Previous: Avoiding the Post-Intubation Crash
Another question is whether volume and pressure are considered modes. The easiest way to describe this is to picture the ventilator as a flow generator. The practitioner may target that flow to a specific volume or a specific pressure. Therefore, when discussing volume or pressure ventilation, it may be beneficial to think of these as flow targets rather than modes. Both volume and pressure ventilation have advantages and disadvantages that will be discussed in upcoming articles.
There are over 174 different names for ventilation modes. Here is just a small sample of names/acronyms of modes from a few leading ventilator manufacturers:
(S)CMV, IPPV, Volume A/C, AC/VC, Volume Control, VCV
P-CMV, P-A/C, BiPAP, Pressure A/C, AC-PC, Pressure Control
Spont, CPAP/P.Supp., CPAP PSV, Spont PSV, Pressure Support CPAP
SIMV, SIMV, SIMV/PS, Volume SIMV, SIMV-VC, SIMV (Volume Control)
P-SIMV, Pressure SIMV, SIMV-PC
APVcmv, IPPV/AutoFlow, PRVC A/C, AC-VC+, PRVC, PCV-VG
APVsimv, SIMV/AutoFlow, PRVC SIMV, SIMV-VC+, SIMV-PCVG
DuoPap, BiPAP, APRV/BiPhasic, BiLevel, Bi-vent, BiLevel
Trying to navigate through this perplexing sea of acronyms is a daunting task to say the least. Many of these modes are exactly the same or very similar but are labeled differently as manufacturers attempt to reach a product differential in an extremely competitive market. The advent of microprocessor technology has allowed a single ventilator to produce any number of output waveforms, some as limitless as the operator’s imagination.3
How do you determine what mode will best benefit a patient? Not surprisingly, modes are often chosen based on the comfort level and experience of the practitioner. This has some advantages if the provider is skilled at making critical adjustments to the ventilator settings to improve the oxygenation and ventilation. Knowing how the patient is likely to respond to even subtle changes in a particular mode goes a long way in safely managing a mechanically ventilated patient.
First and foremost, the practitioner must understand the modes available on their ventilator, as well as the available flow from which the patient can draw a spontaneous breath. Typically, turbine or blower driven ventilators can produce greater flows, which can be beneficial to the “air hungry” patient or patients with a high minute volume demands.
Related: The Importance of Head Positioning During Endotracheal Intubation
When transferring a patient from a hospital ventilator to a transport ventilator, it is important to match the settings as equally as possible to obtain adequate oxygenation/ventilation status. It is wise to incorporate a discussion at bedside with the respiratory therapist, nurse, and physician, if possible, prior to transferring the patient to the transport ventilator. Settings such as inspiratory time, inspiratory to expiratory ratio, sensitivity, P-ramp or rise time are not often discussed during the initial transfer but should be matched as closely as possible to facilitate a smoother transition and optimal patient comfort.
Here are some of the most common modes used today:
Assist Control or A/C: The patient will receive mandatory breaths at a set respiratory rate, inspiratory flow, and either volume or pressure target. The patient may trigger a breath in between the set rate and that would cause them to receive either the volume or pressure target set on the ventilator. In this mode each breath delivered would be of the same volume or pressure. The most common settings to match in A/C mode are respiratory rate, tidal volume, inspiratory time or inspiratory to expiratory ratio, PEEP, FiO2 and sensitivity.
Example of assist control with patient-triggered breath
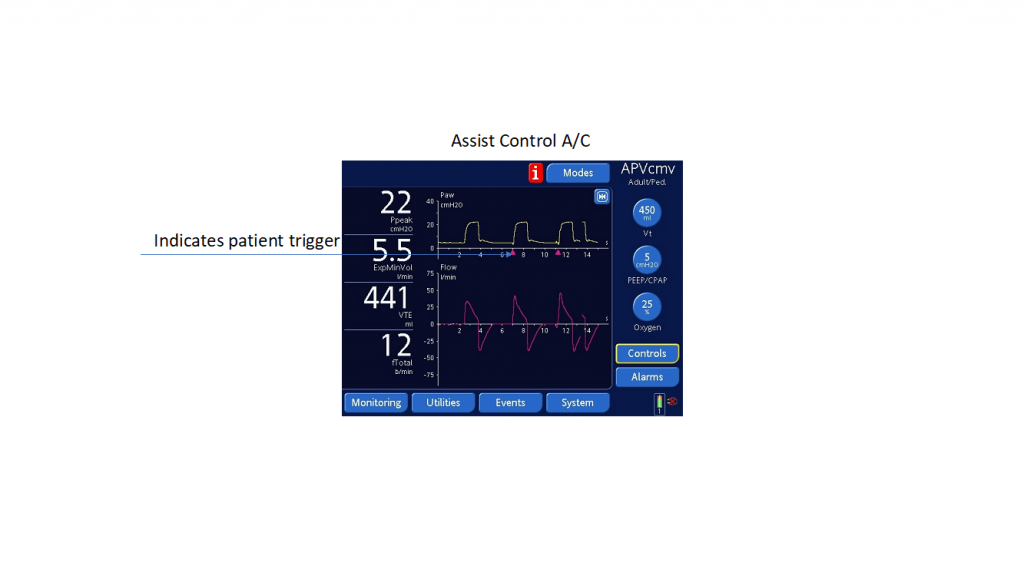
Note: The purple triangle indicates a patient-initiated breath delivering the set target tidal volume. (Photo courtesy of Vent-Pro Training)
Synchronized Intermittent Mandatory Ventilation or SIMV: The patient will receive mandatory breaths at a set respiratory rate, inspiratory flow, and either volume or pressure target. The patient may breathe in-between the scheduled breaths. Their spontaneous breaths can vary greatly depending on patient effort, lung compliance and airway resistance. It is advisable to add a pressure support breath to an SIMV mode. This pressure support breath acts as a “boost” breath to overcome added airway resistance within the circuit and the respiratory tract. The exhaled tidal volume from the pressure support breath varies greatly and titrating the applied pressure for a desired volume warrants attention. It is important to note that pressure support has no inspiratory time or set respiratory rate; it is only activated when the patient takes a spontaneous breath. Some of the more sophisticated transport ventilators allow for adjusting when the flow terminates the breath. It may be time cycled or flow terminated after a set percentage of the expiratory flow.
Example of SIMV mode with spontaneous breath:
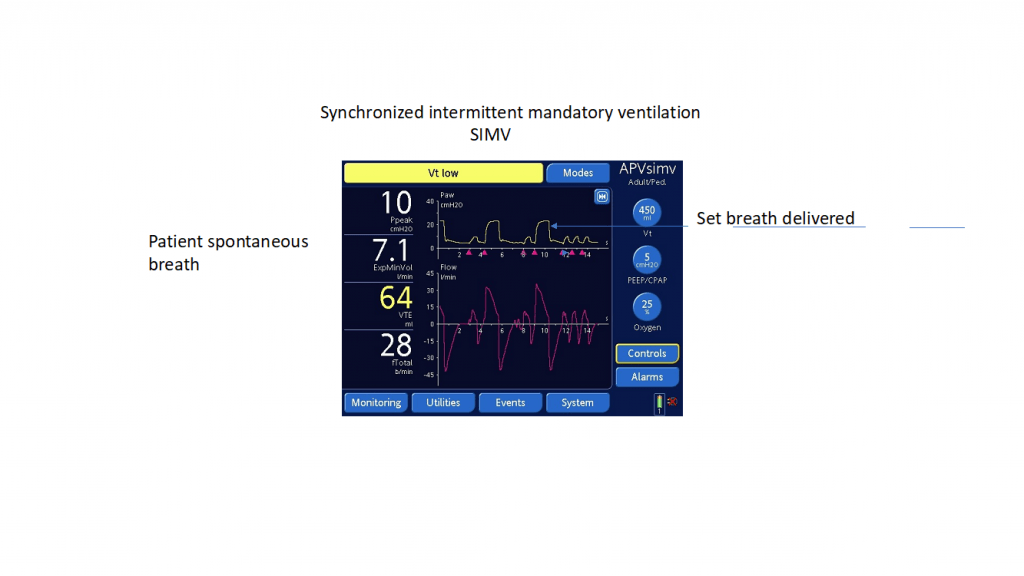
Note: The purple triangle indicates patient’s spontaneous breath. Compare the pressure tracing to the delivered breath. (Photo courtesy of Vent-Pro Training)
Continuous Positive Airway Pressure or CPAP: This mode provides a continuous elevated baseline pressure during spontaneous breathing. There may be some confusion when discussing PEEP and CPAP. Typically, PEEP is an elevated baseline pressure during mechanical ventilation whereas CPAP is elevated baseline pressure during spontaneous breathing. In other words, PEEP is a setting on the ventilator whereas CPAP is a mode of ventilation.3
Example of CPAP:
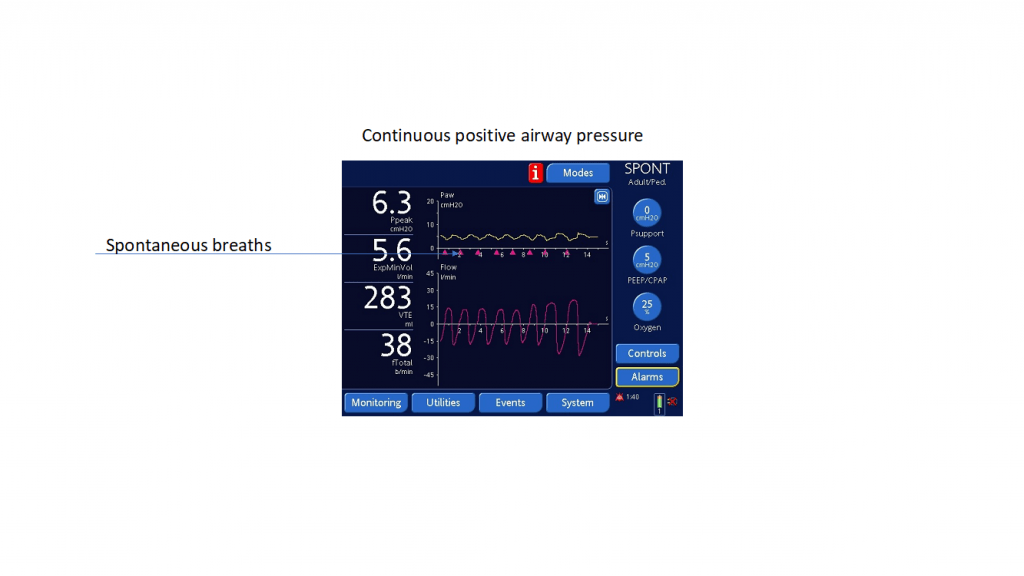
Note: All spontaneous breaths during CPAP mode. (Photo courtesy of Vent-Pro Training)
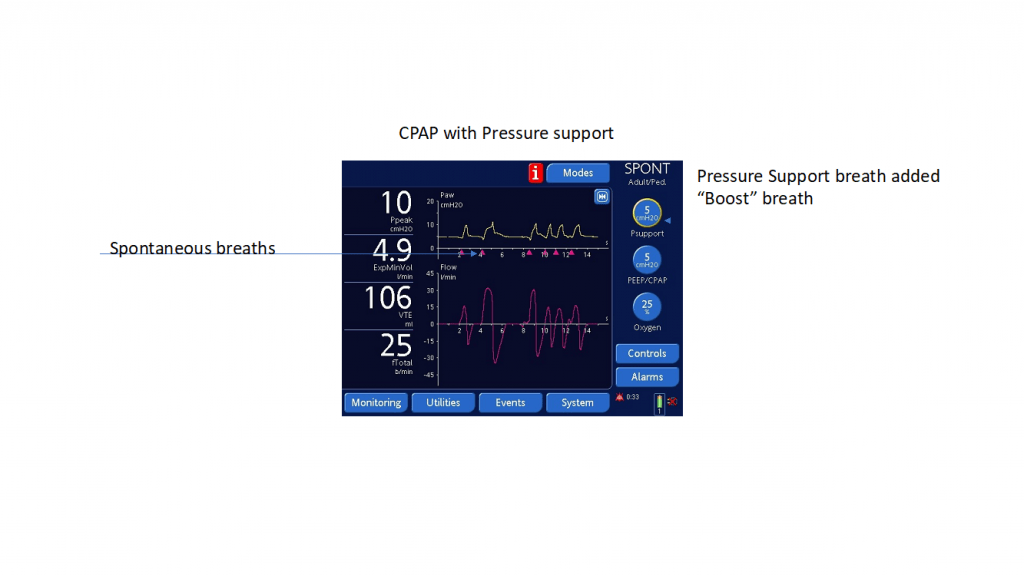
Note: All breaths are patient dependent. Pressure support can be added to assist the patient to decrease the work of breathing. (Photo courtesy of Vent-Pro Training)
Related: Training Tips for CPAP and BiPAP
In this brief article, several different modes of ventilation typically available in mid-level transport ventilators have been discussed. They are assist control with a volume or pressure target, synchronized intermittent mandatory ventilation with a volume or pressure target, and CPAP with or without a pressure support breath added. For safe transport of a patient on a mechanical ventilator, it is wise to keep things as simple as possible. When choosing a mode that will best match the patient’s needs consider safety and comfort as your main priorities. There are environmental factors that influence choice of mode during transport such as patient stimulation, temperature, and comfort level of the transport stretcher. Engage all available resources when developing a strategy for the mission. Finally, vigilant monitoring of patient synchrony with the ventilator during transport is crucial. Always have a plan “B” in place for any unforeseen circumstances.
References
- Cheifetz, I., MacIntyre, N., Marini, J., editors. (2017) Mechanical Ventilation: Essentials for Current Adult and Pediatric Practice. Society of Critical Care Medicine: Mount Prospect, Illinois
- Chang, D., editor. (2006) Clinical application of mechanical ventilation, 3rd edition. Delmar Thomson Learning: New York, New York.
- MacIntyre, N., Branson, R., editors. (2009) Mechanical Ventilatio. Saunders Elsevier: St. Louis, Missouri
Michael Schauf, RRT-NPS, has been a registered respiratory therapist at Albany Medical Center Hospital in New York since 1994. He covers all in-patient units, ICUs, the adult and pediatric Emergency Departments and is a member of the neonatal/pediatric transport team at this Level I Trauma and Level 3 NICU Center. Michael is the founder of Vent-Pro Training, teaching medics and nurses around the world how to manage mechanically ventilated patients during ground, rotor, and fixed-wing transports. He has been a flight respiratory therapist since 1998, currently working for AirMed and as a clinical education specialist for AMR. Michael authored the respiratory chapter of, “Critical Care Transport, 2nd edition,” published by Jones & Bartlett and is an adjunct instructor in the Respiratory Care Program at Hudson Valley Community College.


Recent Comments