Photo/Rick McClure
In earlier columns, use of CPAP and/or BiPAP to treat respiratory distress was described as both an art and a science. The art of using non-invasive ventilation (NIV) involves recognizing the need, selling NIV to your patient, and knowing when to quit. NIV science describes the ability to size a mask, select initial settings and titrate pressures. Training helps improve skills in both the art and science of using CPAP or BiPAP to improve patient outcomes.
One of the first and most valuable aspects of training on NIV is trying it yourself. For virtually any positive pressure respiratory device or ventilation mode, trying it yourself is a far superior teacher compared to simulation. Disposable CPAP and BiPAP units can be cleaned between uses in a similar fashion to cleaning CPR mannequins. Try various pressure settings and, if you use in-line nebulizers, try some nebulized saline solution. It’s also helpful to try starting CPAP at various pressures. Some experts suggest starting as low as 2 to 3 CWP and titrating upwards for comfort. Once you have the experience of wearing CPAP at various flows, you should try turning the gas off to get a feeling for the anti-asphyxia features of the device. A single practice session should give you an immediate sense of the impression most dyspneic patients get from being handed a loud, windy mask to put over their face. It can be very intimidating.
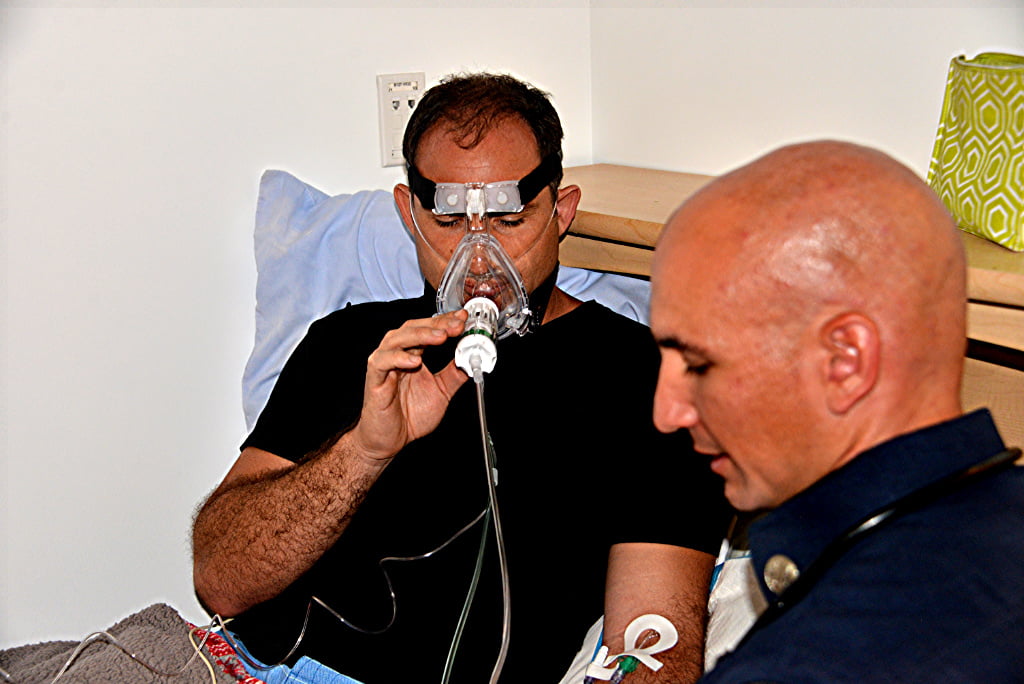
After you’ve had opportunity to try CPAP and/or BiPAP yourself, you should practice applying CPAP to a colleague. The CPAP mask should always be handed to the patient so that they can place it on their face by themselves, which is far less frightening than having a stranger push it into place. Adjusting pressures so your “patient” is comfortable can provide valuable, real-life experience. Once comfortable, the skill of getting the head strapping system attached to the mask and into the proper place on the head is a must. Nearly every system has nuances that are best learned during practice than when actually needed.
Practice is also needed in sizing masks on people with different faces and body builds. CPAP and BiPAP equipment, including disposables, require multiple steps to set up and operate. EMS providers should be fluent in quickly unpackaging, assembling, connecting and deploying NIV. Practice sealing a mask, recognizing and troubleshooting significant leaks, and using nasal cannula capnography under the NIV mask are very helpful.
Practicing the combined art and science of knowing when to quit CPAP or BiPAP can include real scenarios with varied respiratory rates, tidal volumes and other measurable parameters to present cases for discussion.
While they may seem simple, neither CPAP nor BiPAP are frequently used pieces of equipment. In fact, the low frequency with which NIV is used in the prehospital environment cries out for more frequent re-familiarization and routine practice sessions. Managing an acutely dyspneic patient with confidence and speed can majorly affect outcomes. Practice pays off.
References
- Liesching T, Kwok H, Hill NS. Acute applications of noninvasive positive pressure ventilation. Chest 2003; 124:699.
- Myers JB, Slovis CM, Eckstein M, Goodloe JM, Isaacs SM, Loflin JR, Mechem CC, Richmond NJ, and Pepe PE. Evidence-Based Performance Measures for Emergency Medical Services Systems: A Model for Expanded EMS Benchmarking. Prehospital Emergency Care. 2008;12:141-151.
- Kosowsky JM, Stephanides SL, Branson RD, et al. Prehospital use of continuous positive airway pressure (CPAP) for presumed pulmonary edema: A preliminary case series. Prehosp Emerg Care. 2001;5:190–196.
- Craven RA, Singletary N, Bosken L, et al. Use of bi-level positive airway pressure in out-of hospital patients. Acad Emerg Med. 2000;7:1065–1068.
- Hubble MW, Richards ME, Jarvis R, Millikan T, Young D. Effectiveness of prehospital continuous positive airway pressure in the management of acute pulmonary edema. Prehosp Emerg Care 2006;10(4):430–9.
- Alexander JL. Use of continuous positive airway pressure in rural emergency medical services systems for acute pulmonary edema. Acad Emerg Med. 2006;13(5 suppl 1):S66.
- Peter JV, Moran JL, Phillips-Hughes J, et al. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary edema: A meta-analysis. Lancet. 2008;367(9517):1155–1163.
- Winck JC, Azevedo LF, Costa-Pereira A, et al. Efficacy and safety of non-invasive ventilation in the treatment of acute cardiogenic pulmonary edema—a systematic review and metaanalysis. Crit Care. 2006;10:R49.
Mike McEvoy, PhD, NRP, RN, CCRN, is the EMS coordinator for Saratoga County, New York, and the professional development coordinator for Clifton Park and Halfmoon Ambulance. He is a nurse clinician in the adult and pediatric cardiac surgery intensive care units at Albany Medical Center, where he also teaches critical care medicine. McEvoy is the chief medical officer and firefighter/paramedic for West Crescent Fire Department in Clifton, New York. He is also the chair of the EMS Section board of directors for the International Association of Fire Chiefs and a member of the New York State Governor’s EMS Advisory Council. He is a lead author of the textbook Critical Care Transport, the “Informed” Pocket References (Jones & Bartlett), and the American Academy of Pediatrics textbook Pediatric Education for Prehospital Professionals (PEPP).


