This picture shows noninvasive training session with a Revel transport ventilator. (Photos provided by the author, seen on the right.)
You are dispatched to a 69-year old male patient with difficulty breathing. He presents with tripoding and is able to speak only in half sentences. He fails your “look” test and your EMT partner quickly connects him to your monitor while you do a quick assessment to establish a strategy to help this struggling patient. His breathing is pursed lipped and uses accessory muscles with obvious intercostal retractions. Breath sounds are diminished bilaterally. There are fine crackles in the bases with faint expiratory wheezes in the apices and scattered rhonchi in the right lower lobe.
The monitor reveals HR 122, BP 145/90, respiratory rate 25 bpm, and a pulse oximetry reading of 81% on room air. His temperature is 101.9°F. You start a nebulized albuterol treatment via face mask while you contemplate your next move. The oxygen saturation slowly climbs to 86%. As you look around the room, you see multiple MDI metered dose inhalers medications strewn about and an oxygen concentrator in the corner of the room. The entire room smells like an ash tray, and the patient confirms he has emphysema and still smokes.
You have a half hour ride to the nearest hospital. After assessing the patient’s ability to tolerate a CPAP mask, you decide to go the noninvasive ventilation (NIV) route and place the patient on 8 cmH2O CPAP via full face mask with another albuterol nebulizer running. The saturation climbs to 89%. As you are loading the patient into the rig, your fresh-out-of-school partner asks: “Why not BiPAP?” You look at her and say: “Good question.” On arrival in the hospital, the respiratory therapist readies a BiPAP setup. So, why not a BiPAP for transport?
Demonstrating the differences between CPAP and BiPap.
Let’s first look at this scenario in detail and discuss our options. On initial assessment you found a patient in respiratory distress, neither oxygenating nor ventilating effectively. The wheezing, rhonchi, and crackles are certainly contributing factors to his condition. He confirmed he has emphysema and is supposed to be on home oxygen but appears non-compliant and admits to still smoking. This raises some issues.
To address oxygenation in the prehospital environment, we typically administer oxygen using a nasal cannula or non-rebreather mask (NRBM) to hopefully correct hypoxia. In this scenario, oxygen administration may increase the pulse oximetry reading, but do very little to lower the patient’s work of breathing (WOB), which is the ventilation portion of the problem.
Using a low threshold for intubation in this particular patient may not be wise, given the obvious risks involved. Noninvasive ventilation will augment alveolar ventilation, improve oxygenation, increase lung volume, and unload respiratory muscles.1 However, it is critical to assess the patient for contraindications prior to applying NIV. These include:2
Absolute Contraindications
| The need for emergent intubation (Cardiac or Respiratory arrest) |
| Severe Respiratory Distress |
| Unstable cardiac arrhythmia |
Relative Contraindications
| Non-respiratory organ failure that is not acutely life-threatening |
| GCS < 10 |
| Severe upper gastrointestinal bleeding |
| Hemodynamic instability |
| Facial or neurological surgery, trauma, or deformity prohibiting a mask seal |
| Significant airway obstruction |
| Inability to cooperate, protect airway, or clear secretions |
| Anticipated prolonged need for mechanical ventilation (> 4-7 days) |
| Recent esophageal or gastric anastomosis |
| Severe anxiety issues coupled with claustrophobia |
By choosing CPAP for NIV, you are setting a positive end expiratory pressure (PEEP) to decrease both the opening pressure of the airway units and development of atelectasis.1 This CPAP pressure is applied across the respiratory cycle (both the inspiratory and expiratory phases). However, the amount of tidal volume exhaled is patient dependent. Therefore, one could consider BiPAP to increase the tidal volume (Vt) and decrease the work of breathing (WOB).
Think of BiPAP as two levels of pressure. The lower pressure is the CPAP/PEEP level, referred to as EPAP (expiratory positive airway pressure). The upper pressure is referred to as IPAP (inspiratory positive airway pressure) and is applied by adding a pressure support breath. Typical BiPAP settings can range from 10/5 to 20/5 and the wider the pressure gradient (delta p) the larger expected exhaled tidal volume.
Pressure/Time Scalar for CPAP/BiPap
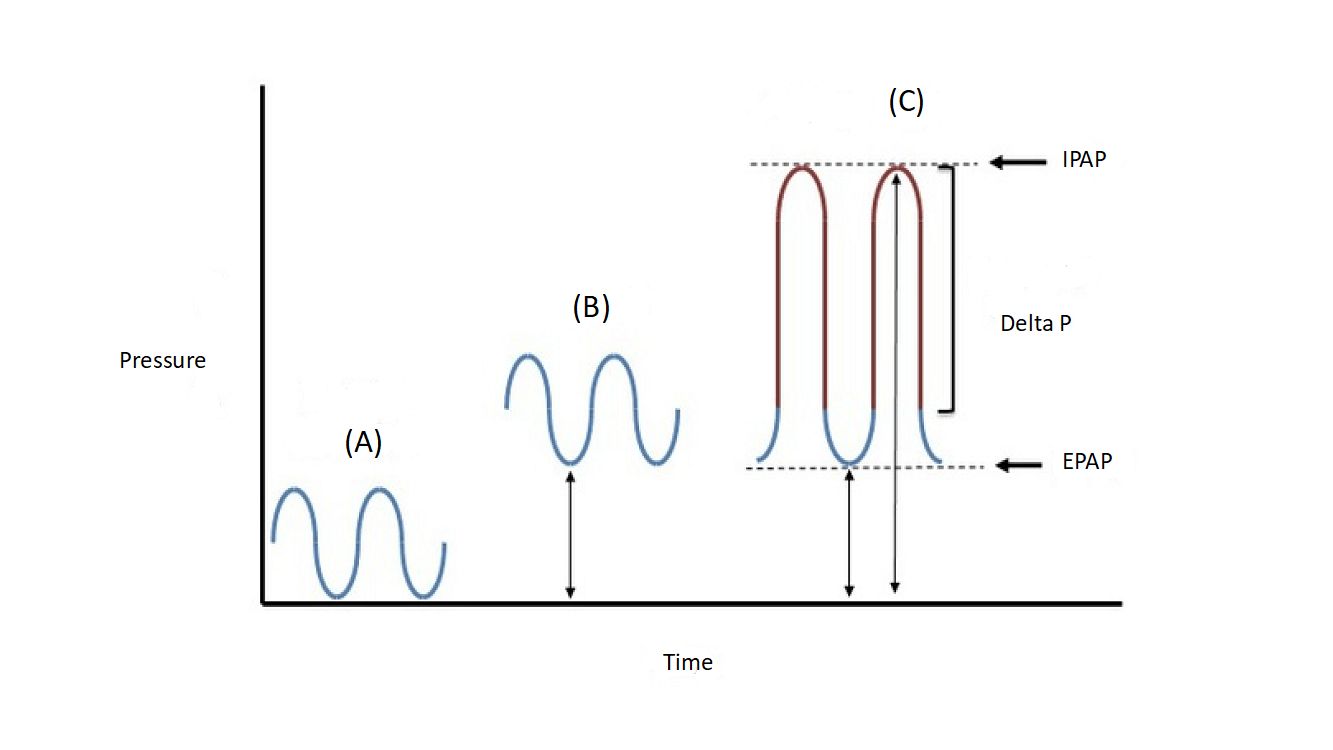
(A) Normal Breathing (B) CPAP (C) BiPap
IPAP Inspiratory positive airway pressure
EPAP Expiratory positive airway pressure
It is extremely important to understand how your equipment delivers the pressure. Some devices are simply connected to a 50 psi oxygen outlet and have preset pressures. Some ventilators allow BiPAP setting a respiratory rate and a peak inspiratory pressure, or a pressure above PEEP (PIP or PAP) with an inspiratory time (It) attached to it. This pressure is different from the pressure support breath which has no inspiratory time attached to it and is often referred to as a “boost” breath. The other major concern is the maximum flow available to the patient. Some transport ventilators are piston driven and may deliver approximately 60-120 liters per minute of flow, whereas a turbine driven ventilator may deliver approximately 160-240 liters per minute. This is important when the BiPAP settings are on the high side (20/10) and there are inherent leaks with noninvasive ventilation. Couple these with a patient breathing in the mid-twenties, and the flow may be insufficient.
Multiple experts suggest that NIV should be considered as the first choice of therapy for any patient in respiratory distress presenting to the emergency department. But many factors go into the equation for deciding between CPAP and BiPAP. It is commonplace to start with BiPAP settings of 10/5 and titrate the FiO2 for sats > 92%. This is followed by a chest x-ray (CXR) and an arterial or venous blood gas (ABG or VBG) to obtain baseline oxygenation/ventilation status. From these results, adjustments are made as necessary. Caution must be taken not to induce breath stacking in the tachypneic patient as that readily leads to air-trapping. In the author’s experience, some patients oxygenate and ventilate better on CPAP than BiPAP. Every patient should be treated individually and no “cookbook” strategy works for everyone.
In the prehospital setting, CPAP has been found just as beneficial as BiPAP in terms of meaningful outcomes, including short term mortality.3 The decision to use CPAP versus BiPAP should be discussed with medical control if there is a long transport time. Any potential adjustment parameters should be determined prior to departure, as sometimes small adjustments in settings may make a difference in patient compliance. Vigilant assessment of the patient’s respiratory status is paramount. Always consider patient safety and monitor patient synchrony with the delivery device.
References
- Ira Cheifetz, Neil MacIntyre, John J. Marini Mechanical Ventilation: Essentials for Current Adult and Pediatric Practice, Society of Critical Care Medicine. 2017.
- Adapted from: International Consensus Conference in Intensive Care Medicine: Noninvasive positive pressure ventilation in acute respiratory failure. Am J respire Crit Care Med 2001; 163;283.
- Gray A, Goodacre S, Newby D, et al. Noninvasive Ventilation in Acute Cardiogenic Pulmonary Edema. N Engl J Med, 2008; 359: 142-151.
Michael Schauf, RRT-NPS, has been a registered respiratory therapist at Albany Medical Center Hospital in New York since 1994. He covers all in-patient units, ICUs, the adult and pediatric Emergency Departments and is a member of the neonatal/pediatric transport team at this Level I Trauma and Level 3 NICU Center. Michael is the founder of Vent-Pro Training, teaching medics and nurses around the world how to manage mechanically ventilated patients during ground, rotor, and fixed-wing transports. He has been a flight respiratory therapist since 1998, currently working for AirMed and as a clinical education specialist for AMR. Michael authored the respiratory chapter of, “Critical Care Transport, 2nd edition,” published by Jones & Bartlett and is an adjunct instructor in the Respiratory Care Program at Hudson Valley Community College.


