
Photo provided by the author.
You should read this article because of the following possible scenarios:
- You are dispatched to a nursing home/rehabilitation center for a 73-year-old man on a mechanical ventilator with a decreased level of consciousness.
- You are dispatched to a residence for a nine-year-old girl on a mechanical ventilator who is having trouble breathing.
- An ambulance from a different agency has been involved in an accident while traveling through your first due area. You respond and find the care provider has been injured and the patient is on a ventilator.
Maybe ten years ago, none of these scenarios would have been realistic as it was uncommon for a person on a ventilator to live at home. The number of patients requiring long-term mechanical ventilation, however, is increasing. One reason is that improved EMS and intensive care unit (ICU) care has resulted in many patients surviving episodes of acute respiratory failure, which potentially results in a longer time on mechanical ventilation during convalescence. Another reason is that mechanical ventilation is increasingly being used as a therapeutic option for patients with conditions such as symptomatic chronic hypoventilation.1
Related: Mechanical Ventilation During Out-of-Hospital Cardiac Arrest
Further, there are continuing efforts by ventilator manufacturers to make home ventilators more accessible and user friendly. These factors, along with others, demonstrate that there will be a continuing increase in the number of patients receiving home mechanical ventilation in the United States. Consequently, it is now entirely possible for you to be called to a location outside of a hospital to assist a patient on a mechanical ventilator, whether the emergency is associated with the ventilator or completely unrelated.
The purpose of this article is by no means meant to qualify or credential you in the use of a mechanical ventilator. The goal is to provide a basic overview and improve your understanding of a mechanical ventilator in order to increase your comfort level in the event you walk into a home and find that your patient is on a ventilator. It should also be noted that this article in no way endorses or promotes the use of any specific brand of ventilator.
Why Would a Ventilated Patient Be at Home?
Mechanical ventilation in the home is not a completely new idea. Remember the tank respirator, or iron lung, on which many polio patients were dependent in the early 1900s. Physicians who treated people in the acute, early stage of polio found that many patients were unable to breathe because the virus paralyzed the muscle groups in the chest. Death was frequent until a negative pressure tank respirator was developed that could maintain respiration artificially until a person could breathe independently. Later, positive pressure replaced negative pressure in ventilator use.
Pediatric patients became the next target population for home mechanical ventilation, with the Medicaid Katie Beckett Waiver serving as an important landmark.2 Today, there are multiple conditions for which a patient could be living in your response area on a mechanical ventilator, ranging from neurological to cardiovascular to musculo-skeletal. Table 1 lists some examples but is certainly not comprehensive.
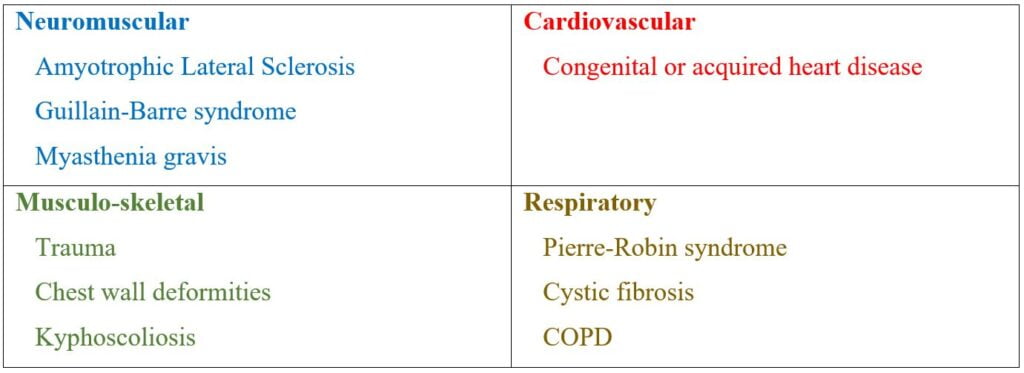
Table 1
The Mechanical Ventilator
In its simplest form, a mechanical ventilator can be compared to an air compressor, it draws air in from the atmosphere via an opening, then propels it out through another port to the patient. Any given patient will be on either a volume or pressure setting, meaning that the patient’s lungs are being inflated to either a preset tidal volume or a preset pressure.
Related: Optimal Prehospital Airway Management Depends on EMS System Efficiency
Normally, a ventilator would be seen connected to an oxygen source, but if a patient is set at 21% oxygen, the same as the atmosphere, then no additional cylinder is needed. In addition to the air intake and port leading to the patient, the machine may also have an air intake for cooling and a port for bleeding off expired air. All of these orifices should be kept unobstructed. Power is supplied from either a wall outlet or internal batteries. Some may have additional external batteries.
When looking at a ventilator in use, you can think of it as having five components. Beginning at the patient, you will see:
1) An airway device such as an ET or tracheostomy tube,
2) There may then be a disposable humidifier and/or bacterial filter, (the filter may alternatively be between the ventilator and the circuit),
3) The circuit, which is the flexible tubing running from the patient to the ventilator,
4) The ventilator, and
5) A high- or low-pressure-hose connected to an oxygen cylinder.
The screen of the ventilator may appear complicated, but like other equipment, it can be broken down. For emergent purposes, the first thing you should check is what mode the patient is on, and a helpful tip is that oftentimes, the name of the mode explains exactly what it does, for example, in assist/control, if the patient takes a breath, the ventilator assists with it, if the patient is not taking any breaths, the ventilator will control them.
You should also understand the difference between control and support. In any control setting, the ventilator is initiating all the breaths, or controlling them, in a support mode, the patient is breathing and the ventilator is supporting these breaths. There are of course, modes in which it is not as self-explanatory, such as synchronized intermittent mandatory ventilation (SIMV) or pressure regulated volume control (PRVC). There are multiple sources that explain the modes and settings of ventilation more thoroughly, such as In-Depth Overview of Mechanical Ventilation.3
It will also be helpful to remember that all the basic principles of manual ventilation still apply to mechanical ventilation, including tidal and minute volume, rate, PEEP, and inspiratory time.
What Could Go Wrong?
When initially approaching a patient on a ventilator who is in distress, you will need to determine whether the problem lies with the patient or with the ventilator as soon as you can. Again, in this context, we are addressing the ventilator.
The problems associated with mechanical ventilation can probably be placed in one of three categories, the airway, the circuit or the ventilator. The potential issues that may occur with the airway are very similar to problems that may affect the circuit. The ET or tracheostomy tube may become obstructed, typically by fluid, sputum or kinking. The circuit can experience the same problems plus it can inadvertently be disconnected from the ET tube or the ventilator. All of the plastic components, including the circuit, filters and humidifiers are disposable and can be replaced if they were found to be clogged, broken or otherwise compromised.
If a spare is not available, the filter and humidifier can still be removed and left out temporarily. A clogged or damaged circuit would need to be replaced immediately. A clogged ET tube or circuit will cause a high-pressure alarm on the ventilator, a disconnection or other leak will result in a low-pressure alarm. It is possible for the problem to be the ventilator, but it should be noted that mechanical ventilator malfunctions are extremely rare.
Related: It’s About Paramedic Intubation Skill Maintenance, Not ETI vs. SGA
One possible complication can be if the ventilator lost power or was shut off. Many ventilators allow you to select either a “new” or “same” patient setting. If the ventilator was shut off or lost power and then turned back on, it is possible that the patient was placed in the incorrect mode or settings. This could cause issues such as excessive or inadequate tidal volume, or excessively long or short inspiratory time. If you arrived to find a ventilator completely off, see if you can turn it on and select “same patient” as this should reset the patient’s correct settings.
If you must help a caregiver reset settings, the most important action is to first select the correct mode. Once a mode is selected, many ventilators only let you adjust the settings that are applicable. For example, if you place a ventilator in pressure support, you will be given the option of changing pressure support, PEEP, and oxygen concentration only, you won’t have to worry about setting a volume or a rate because these buttons will not be active.
Ideally, someone on the scene will have the patient’s settings for you to refer to, or there should be an emergency number to call, similar to an LVAD patient. If no settings are available, you are not comfortable in selecting them, or the patient is remaining in any degree of discomfort, they should be managed manually with a bag vale mask and transported to the hospital.
Management Pearls
- Assess the patient, remember the DOPE mnemonic; Displacement: assess for displacement (right mainstem) or dislodgement of the ET tube, Obstruction: check for a mucus plug or kink in the ET tube or circuit, Pneumothorax: assess bilateral breath sounds, Equipment: look for any problems with the ventilator. For patient problems, obviously examine and focus on the patient.
- Disconnect the patient from the ventilator and manually ventilate using a BVM. Assess lung compliance. If the patient is not difficult to ventilate the problem may be with the ventilator or the circuit. If the patient is difficult to ventilate, it may be a problem with the patient or the endotracheal/tracheostomy tube.
- For ET tube or circuit problems, check them both for obstruction or kinking. A suction catheter can be passed through the ET tube to check its patency.
- For ventilator problems, check for correctable causes, such as a disconnected power cord or circuit, and verify that the ventilation mode and settings are correct.
- Remember that if the problem is the ventilator, or if you are in doubt, BVM ventilation is your fail-safe.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4561264/
- https://portal.ct.gov/-/media/Departments-and-Agencies/DSS/OLCRAH/OperationalPolicyKatieBeckettWaiver.pdf?la=en
- https://www.jems.com/patient-care/depth-overview-mechanical-ventilation/
John Alexander, MS, NRP, CNA, is a paramedic with Lifeline Air and Ground Transport Service at The Johns Hopkins Hospital in Baltimore. He is a retired fire and EMS captain from the Anne Arundel County Fire Department and has been a paramedic for over thirty years.


Recent Comments