
To improve prehospital medicine and patient outcomes, EMS requires support from the medical community, the authors write. (Photo provided by the authors.)
We would like to comment on the prehospital airway debate at the 2020 NAEMSP Annual Meeting.
Prehospital endotracheal intubation (ETI) is being held to low standards. The 2015 Committee on Accreditation of Educational Programs for the Emergency Medical Services Professions (CoAEMSP) standards make it possible for paramedic students to graduate without intubating a live patient.1 For many paramedics, ETI is a rarely performed skill,2 leading many to question if prehospital providers should continue to provide this potentially life-saving skill.
The 2019 Rhode Island (RI) Emergency Medical Services (EMS) report on unidentified esophageal intubation intensified this debate. Although most of the misplaced ETI tubes were placed by emergency medical technician (EMT)-cardiacs—a lower-tier advanced life support (ALS) provider unique to RI—the lack of procedural competence and associated mortality renewed the public debate over prehospital ETI.3 This debate goes beyond intubation for cardiac arrest. For instance, the National Association of EMS Physicians (NAEMSP) set high standards for paramedics and medical directors for EMS systems performing rapid sequence intubation (RSI).4 Why shouldn’t these standards apply to ETI in general?
Airway and System Proficiency
Paramedic skill proficiency for technical procedures such as ETI should be vital considerations for any EMS system. Despite this, EMS systems continue to add paramedics without regard to associated skill dilution.5,6 Estimates have shown that two to 20 percent of calls require ALS interventions, where the majority of patients could be handled by basic life support resources.7,8 Manikin training may support initial and continuous ETI proficiency, but claims that Manikin training alone can guarantee proficiency are either antiquated or based off anecdote.9-11 The International Association of Fire Fighters’ Emergency Medical Services: A Guidebook for Fire-Based Systems conjectures that single-tier ALS systems prove better than multi-tiered systems because of communication simplification and perceived minimal expenditures. However, it offers no evidence that such systems lead to optimal patient outcomes.12 Should the recent RI ETI report and other single-tier ALS systems with questionable ETI performance and outcomes challenge this model?3,13-15 Two-tier systems that use targeted ALS response and fewer paramedics for a given population often report better ETI success rates and cardiac arrest outcomes.16
These metrics can be seen as surrogates for overall EMS system performance. The Pragmatic Airway Resuscitation Trial (PART) study demonstrated that in EMS systems with better baseline survival ETI was favored over supraglottic airway insertion.17 The PART study’s conclusion only appears valid in the lower baseline survival EMS systems included in the study. Other data have shown that paramedic experience is associated with better outcomes.18 Sending paramedic providers to nonparamedic-level calls will not increase their experience; it will only decrease their skill proficiency. A more logical and evidence-based approach would be to model our EMS systems after those which have the best outcomes, most of which are two-tiered systems with a relatively small number of paramedics for their population.
Table 1. Comparison of U.S. EMS Systems Based on 2018 Population Estimates, Number of Paramedics, Population/Paramedic (PP), and (PP) Value (PART trial agencies in red).27
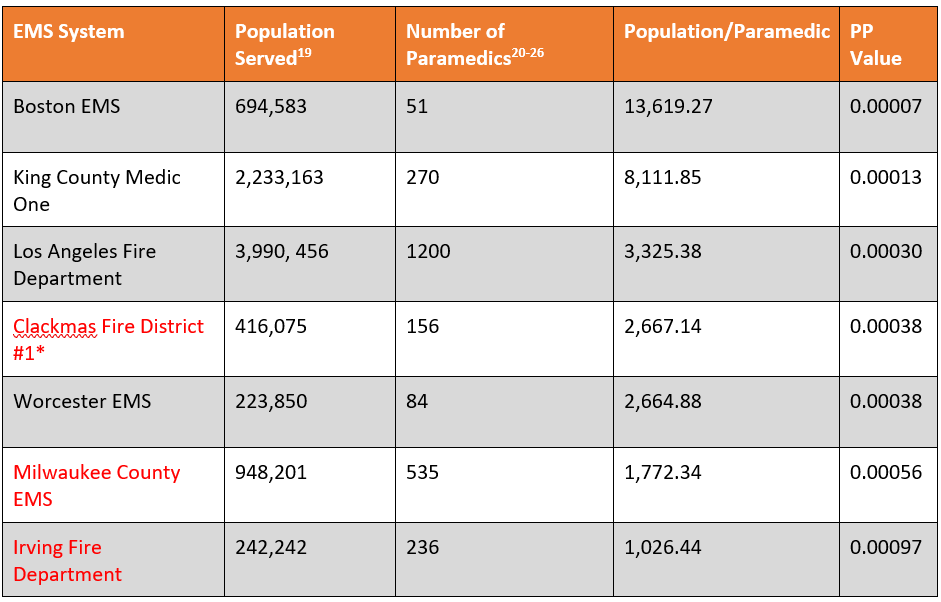
* Does not include paramedics from the county transport provider: American Medical Response
Table 2. Comparison of Various U.S. EMS Systems Based on 2018 Population Estimates, Number of ALS Units, and Population per ALS Unit.
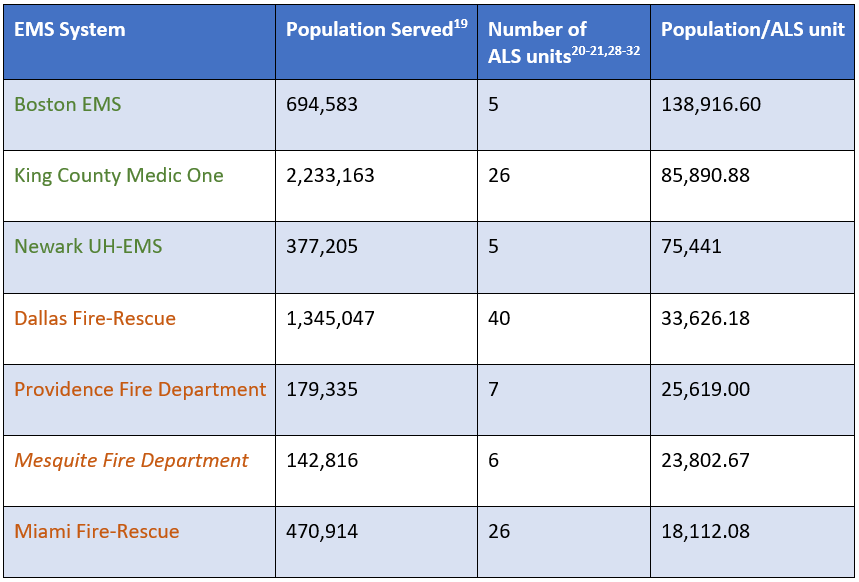
* Two-tier systems are in green and single-tier ALS systems are in orange. PART systems are in italics. (Note: The number of ALS units is based on the standard number of ALS units functioning on a 24-hour basis; peak units are not included. Specialty units and fire apparatus are not included.)
Solutions to EMS System Airway Conundrums
There are various directions leaders can take from this debate. For instance, should states consider certification of need (CON) laws to regulate the number of ALS units or providers? Some ALS interventions are more prevalent than others, e.g., IV access, 12 lead ECG interpretation, analgesia, and so on, and differ in CMS reimbursement. Also, should the paramedic level be divided into high and low tiers, where low-frequency interventions are reserved for the high-tier paramedics? Perhaps the high tier could be a pathway for integrating higher education into ground EMS. Reform depends on the level of commitment from medical, municipal, and regional leaders.
We conclude with the following:
- Skill proficiency is problematic. We see this in other medical fields, so why should EMS be an exception?33-35 We have preliminary data that demonstrates paramedic saturation that is especially prominent in those systems with questionable ETI performance in Tables 1 and 2. With this, we propose a comprehensive analysis of all the PART systems regarding paramedic staffing versus population served.
- Leaders must re-examine their true ALS demands and overlook the “more is better” status quo. Routinely allocating paramedic resources to low-acuity calls is inefficient and not practical.
- The EMS airway debate is only part of a larger discussion: The disparity in quality of prehospital care across the United States. At the 2020 NAEMSP meeting, Dr. Sayre and Dr. Colella illustrated a divergence in EMS capabilities between King County (WI) Medic One and Milwaukee County, Wisconsin. One system allocates significant training and resources to paramedics with support from the regional hospitals and medical school, while the other is constrained by lack of training availability and support from regional medical institutes. This results in one system having superior ETI performance and patient outcomes vs. the other.
To improve prehospital medicine and patient outcomes, EMS requires support from the medical community.
The authors wish to thank Dr. Ryan Pouliot for his input and support in the creation of this article.
References
- CoAEMSP Interpretations of the CAAHEP 2015 Standards and Guidelines for the Accreditation of Educational Programs in the EMS Professions. (n.d.) In Committee on Accreditation for the EMS Professions. Retrieved February 1, 2020, from https://coaemsp.org/?mdocs-file=918.
- Wang, HE, Kupas DF, Hostler D, et al. Procedural experience with out of hospital endotracheal intubation. Crit Care Med. 2005;33(8):1718-1721.
- Arditti, L. (Dec. 3, 2019) EMS Crews Brought Patients to the Hospital With Misplaced Breathing Tubes. None of Them Survived. In ProRepublica. Retrieved February 3, 2020, from https://www.propublica.org/article/ems-crews-brought-patients-to-the-hospital-with-misplaced-breathing-tubes-none-of-them-survived.
- Wang HE, Davis DP, O’Connor RE, et al. Drug-Assisted Intubation in the Prehospital Setting (Resource Document to NAEMSP Position Statement). Prehosp Emerg Care. 2006;10(2):261-271.
- Garza AG, Gratton MC, Coontz D, et al. Effect of Paramedic Experience on Orotracheal Intubation Rates. J Emerg Med. 2003;25(3):251-256.
- Vrotsos KM, Pirrallo RG, Guse, CE, et al. “Does the Number of System Paramedics Affect Clinical Benchmark Thresholds?” Prehospital Emergency Care. 2008; 12(3):302-306.
- Hagiwara S, Oshima K, Aoki M, et al. Does the number of emergency medical technicians affect the neurological outcome of patients with out-of-hospital cardiac arrest? Am J Emerg Med. 2017;35(3):391–396.
- Ryynänen OP1, Iirola T, Reitala J, et al. Is advanced life support better than basic life support in prehospital care? A systematic review. Scand J Trauma Resusc Emerg Med. 2010;18:62
- Stewart RD, Paris PM, Pelton GH, et al. Effect of varied training techniques on field endotracheal intubation success rates. Ann. Emerg. Med. 1984;13: 1032-1036.
- Ludwig, G. (February 1, 2019) EMS: Fewer Paramedics Is Not the Answer. In Firehouse Magazine. Retrieved February 3, 2020 from https://www.firehouse.com/careers-education/article/21036897/ems-fewer-paramedics-is-not-the-answer.
- Hall R, Plant J, Bands C, et al. Human patient simulation is effective for teaching paramedic students endotracheal intubation. Acad Emerg Med. 2005;12(9):850–855.
- Attributes of Fire-Based Systems. In Emergency Medical Services: A Guidebook for Fire-Based Systems. International Association of Firefighters: Washington, DC, pp. 21-27, 2003.
- Gausche M, Lewis RJ, Stratton SJ, Haynes, et al. Effect of Out-of-Hospital Pediatric Endotracheal Intubation on Survival and Neurological Outcome: A Controlled Clinical Trial. JAMA. 2000;283(6):783-790.
- Cobas MA, De la Pena MA, Manning R, et al. Prehospital intubations and mortality: a level 1 trauma centre perspective. Anesth Analg. 2009;109:489–93.
- Davis DP, Hoyt DB, Ochs M, et al. The Effect of Paramedic Rapid Sequence Intubation on Outcome in Patients with Severe Traumatic Brain Injury. J Trauma. 2003;54:444-453.
- Persse DE, Key CB, Bradley RN, et al. Cardiac arrest survival as a function of ambulance deployment strategy in a large urban medical services system. Resuscitation. 2003;59(1):97–104.
- Wang HE, Schmicker RH, Daya MR, et al. Effect of a Strategy of Initial Laryngeal Tube Insertion vs Endotracheal Intubation on 72-Hour Survival in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA. 2018; 320(8):769-778.
- Sayre, MR, Hallstrom A, Rea TD, et al. Cardiac Arrest Survival Rates Depend on Paramedic Experience. Acad Emerg Med. 2006;13(5) Suppl 1: S55-56.
- Population and Housing Unit Estimates. (n.d.) In United States Census Bureau. Retrieved February 1, 2020, from https://www.census.govprograms-surveys/popest.html.
- Boston Emergency Medical Services 2018 Vital Statistics. (n.d.) In City of Boston. Retrieved February 1, 2020, from https://www.boston.gov/sites/default/files/file/document_files/2019/04/2018_boston_ems_vital_stats.pdf.
- Chatalas H, Jacinto T, Azpitarte F, et al. (n.d.) Division of Emergency Medical Services 2018 Annual Report. In King County, WA. Retrieved February 1, 2020, from https://www.kingcounty.gov/depts/health/emergency-medical-services/~/media/depts/health/emergency-medical-services/documents/reports/2018-Annual-Report.ashx.
- About EMS Bureau. (n.d.) In Los Angeles Fire Department. Retrieved January 30, 2020, from https://www.lafd.org/about-ems-bureau.
- Emergency Medical Services. (n.d.) In Clackmas Fire District #1. Retrieved February 1, 2020, from http://www.clackamasfire.com/divisions/emergency-medical-services-division.
- Worcester EMS. (n.d.) In UMASS Memorial Medical Center EMS. Retrieved February 15, 2020, from https://www.umassmemorialems.com/index.php/worcester-ems.
- How’s the System? (n.d.) In Milwaukee County Office of Emergency Management. Retrieved January 30, 2020, from https://county.milwaukee.gov/EN/Office-of-Emergency-Management/System-Status#Emergency_Medical_Services.
- 2017-2018 Irving Fire Department Annual Report. (n.d.) In Irving Fire Department Administration. Retrieved January 31, 2020, from https://www.cityofirving.org/541/Forms-and-Reports.
- Wang HE, Prince D, Stephens SW, et al. Design and Implementation of the Resuscitation Outcomes Consortium Pragmatic Airway Resuscitation Trial (PART). Resuscitation. 2016;101:57-64.
- Find a fire station. (n.d.) In City of Providence. Retrieved February 1, 2020, from http://www.providenceri.gov/fire-department/find-fire-station.
- University Hospital Emergency Medical Services Advanced Life Support. (n.d.) In University Hospital Newark, NJ. Retrieved February 4, 2020, from https://www.uh-ems.net/als.php.
- Find a Fire Station. (n.d.) In City of Dallas. Retrieved February 1, 2020, from https://dallascityhall.com/departments/fire-rescue/Pages/fire-stations.aspx.
- Fire Stations & Coverage. (n.d.) In Official Website of the City of Mesquite. Retrieved February 2, 2002, from https://www.cityofmesquite.com/1327/Fire-Stations-Coverage
- City of Miami Fire-Rescue. (n.d.) In Florida firefighters.com. Retrieved February 1, 2020, from http://www.flfirefighters.com/MiamiFD.htm.
- Adam MA, Thomas S, Youngwirth L, et al. Is There a Minimum Number of Thyroidectomies a Surgeon Should Perform to Optimize Patient Outcomes? Ann Surg 2017;265(2):402-407.
- Fix ML, Enslow MS, Blankenship JF, et al. Emergency medicine resident anesthesia training in a private vs. academic setting. J Emerg Med. 2013;44(3):676–681.
- Maruthappu M, Gilbert BJ, El-Harasis MA, et al. The influence of volume and experience on individual surgical performance: A systematic review. Ann Surg. 2015;261(4):642–647.
Resources
Davis, R. (May 20, 2005) Six minutes to live or die. In USA Today. Retrieved February 1, 2020, from https://usatoday30.usatoday.com/news/nation/ems-day1-cover.htm.
Martin Pelletier, BS, CCEMT-P, FP-C, is a paramedic for Brewster Ambulance in Massachusetts. He also works as a paramedic and SCT-3 provider for Canton Rescue in Canton, NY.
Benjamin Podsiadlo, EMT-P, is the director of clinical integration for Armstrong Ambulance Service in Arlington, Massachusetts.
Stephen Wood, MS, ACNP-BS, is a nurse practitioner and works in emergency medicine at Steward Health System in Massachusetts. He’s a fellow at the Harvard Medical School Center for Bioethics and a contributor for the Petrie-Flom Center blog Bill of Health.
Mark T. Dalton, AAS, BA, EMT-P, is a paramedic and the Director of Operations for Canton Rescue in Canton, NY. He also serves as a member of the North Country Regional Emergency Medical Services Council.





