
All images created by the author.
It’s just the right time of the season to start building back up the bank account after a fun-filled summer. And what better way to do it, than with your longtime partner on a Friday night? You both hop in the rig and head over to grab your favorite Korean barbecue.
You opt to take your food to go but attempt to enjoy a relaxing meal while eating it at the window table in the restaurant. For what seems like the first time in history, you’re able to finish your meal without interruption. You throw away the boxes, say goodbye to the chef, and head out the door to your rig.
As you cross the sidewalk, you can hear the patented CAD chirp inside the unit signaling a call is coming your way, as you await your radio to start chattering about the location and backstory of your next adventure.
Your partner hops into the driver’s seat as you hop into the passenger seat, mark en route and bring up directions.
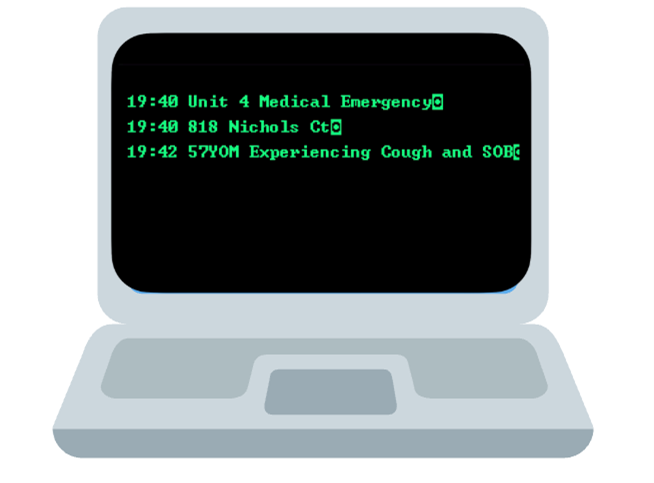
You have approximately a five-minute response time for a 57-year-old male who is experiencing shortness of breath and a cough, according to the caller. It’s a residential home on the backside of town that you never go to.
You arrive on scene to find a one-story rambler tucked back down a short pipestem from the cul-de-sac and a female frantically waving out the front door. You grab your box of life and bag of tricks and head down the pipe stem with your partner.
You meet Kim, the spouse of your future patient, who directs you around back to a detached shed. You notice that the shed has a garage door and as you make your way into the side of the shed, you find your patient lying with his head on his workbench and a bunch of what appears to be plastic and rags around him; you notice a kerosene heater in the corner and a heat gun on the table.
You put your arm out to hold your partner back and ask Kim to open up the garage door to help ventilate. She runs back to get the remote. You look down at your box of life to see if the attached CO monitor has any readings, it does not.
You hear your patient, Marc, coughing, and when doing so, it sounds almost like a weak whimper. You still have not broken the threshold to the side door of the shed as you continue to take in the environment.
You key up the radio, requesting additional resources for environmental monitoring and manpower. You holler over to Marc, asking what’s going on, and he mumbles.
Now that Kim has opened the garage door, you can feel the cool air rushing through the door you’re standing at into the shed. Confirming you’re starting to ventilate the environment.
Kim asks you why you’re not going in to help Marc, and you reassure her that you want to ensure the air is clear in case Marc inhaled toxic fumes, which could be causing his current issues.
You continue to try to dialogue with Marc, only getting mumbling and coughing back. Backup arrives approximately five minutes later with air packs and monitors, and enters, pulling Marc from the environment out onto your cot, as well as providing a gas readout with the only change on their four-gas meter being no change.
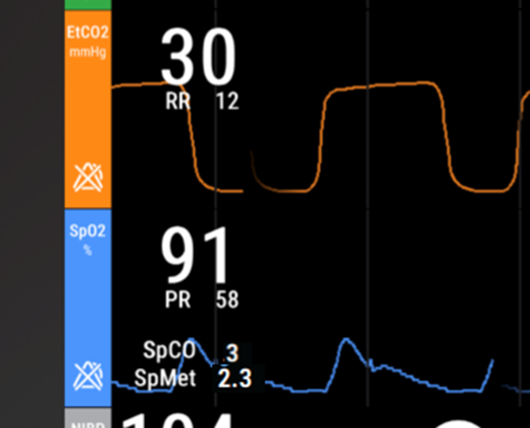
Once on the cot, you quickly get Marc hooked up and find the following.

What are your differentials?
You ask your partner to get Marc‘s lung sounds and find the following. Does this change anything?
You ask the fire crew to see if they can figure out anything else in the room that may have caused this, letting them know you saw rags and burnt plastic in a pile next to the workbench. They step away to assess, and you continue to check out Marc. You look in his airway and find it as follows.
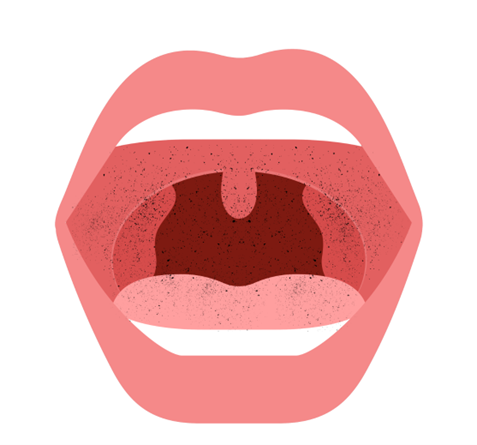
You don’t notice any redness or swelling. You turn to your partner and start discussing the fact that you found the burned plastic in the rags, and the environment had a slight haze and burned plastic odor on your arrival.
Your partner starts the fluid for the pressure and looks back at you, asking if you want oxygen and the CYANOKIT. You shake your head yes, give him a thumbs up as he pulls out the box, and turn back to Marc, trying to coax him into speaking more than just mumbles.
The crew returns, letting you know that all they found was what you had advised them of. It appears that maybe the plastic caught fire or was smoldering, and the rags were placed on top to try to suppress that.
They said there was a heat gun on the table, along with what appeared to be a set of molds used to bend the plastic around. You thank them and let them know you should be good, but if they could double-check with the wife, whose name is Kim, about his medical history and allergies, you would appreciate it.
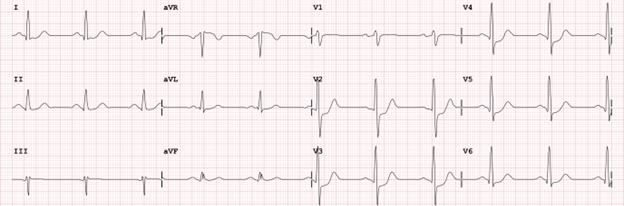
You again turn back to Marc after acquiring your EKG and find the below. Does this change anything?
The crew returns with “Marc is a type 2 diabetic, takes Glucophage, and has no drug allergies.” You thank them and let them know you should be all set.
You turn back to Mark and have a fresh set of vital signs with the bolus of normal saline done and the Cyanokit started. You turn to your partner and let him know, “Let’s head to the university,” and you grab the phone to call in your report. About six minutes into the transport, Marc starts to open his eyes more and moves his hands more but continues to mumble.

How’s he trending?
So, what is going on with Marc, and why did you find him with his head down, mumbling, and his work stuff?
The key to this situation revolves around the causation and events prior to your arrival. You know that last letter E of the SAMPLE history? Mark was heating up plastic, which is a hydrocarbon, to get it to fit around a mold so that it was soft and malleable. When you do that, you release fumes, and in the fumes of hydrocarbons, lives our friend, the hydrogen+ carbon triple bond nitrogen, also known on the street as cyanide.
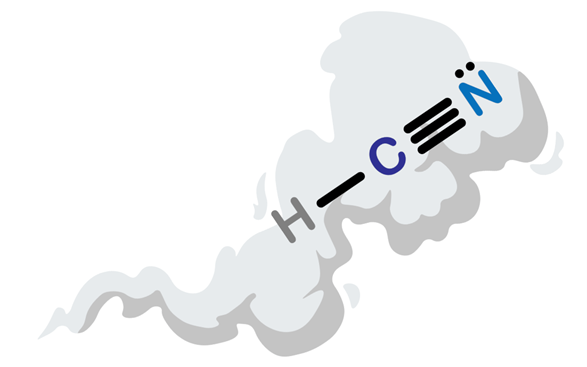
And our concern always with the burning of hydrocarbon is cyanide and to break down the word hydrocarbon in street terms equates to plastics. Whether it is the bottle somebody is smoking crack out of, the couch that their cigarette fell on, the seat in a car and even the PVC or plastic that they’re heating up to make soft and mold around a surface—hydrocarbons=plastics.
Cold smoke fires, ones that don’t have big, hot flames, are the environments and situations we most easily forget to account for cyanide and other toxins in the fumes.

We often associate smoke and fire with thermal injury to the upper airway and swelling, potentially leading to cricothyrotomy. That is always great to keep high in your differential list, but remember it is the upper airway that absorbs the thermal energy.
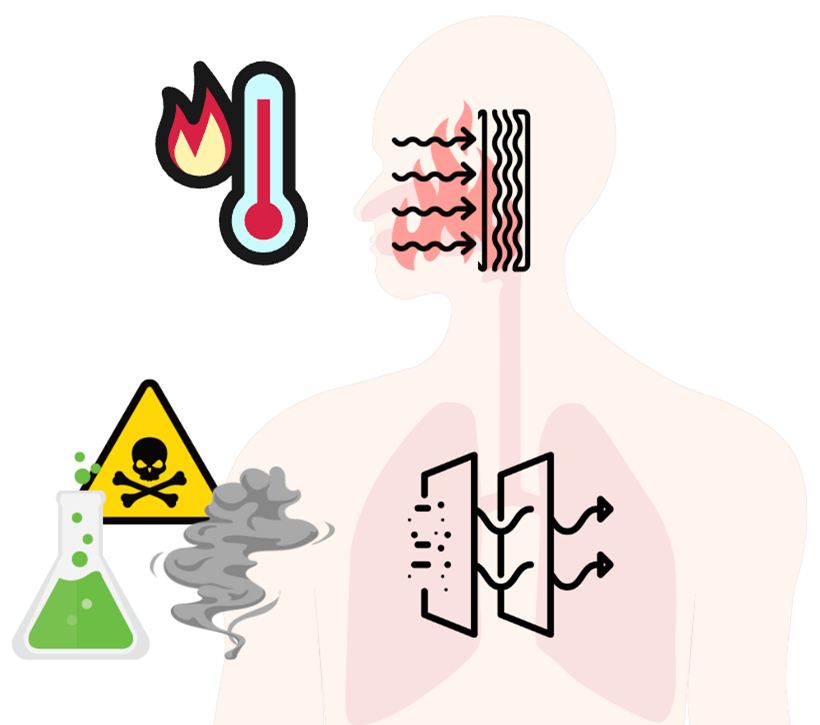
Hence, the swelling, edema and closure. It is the lower airway that filters out the gunk of whatever was Inhaled. The toluene, phosgene the cyanide, the CO, and other products of incomplete combustion, etc.
Depending on the makeup and breakdown of what was inhaled, you can have further problems such as alveolar dysfunction chemical toxicity can damage the alveoli and creates dysfunction where they lose their balloon like affect by breaking down the elastin that gives them the “elastic-balloon” ability.
You can also have the surfactant dry out so gas diffusion across the membrane can be inhibited. These are great patients to not only have your capnography always on but also their carboxyhemoglobin and methemoglobin monitoring too. hooked up because in the acute setting of the pre-hospital environment. Sometimes CO poising isn’t easy to recognize, especially when the situation and environment that caused it isn’t where you find them or they are unconscious and can’t tell you.
So, what was Marc‘s biggest problem? His airway looked fairly clear, his mentation was low, his vital signs presented on the side of lower perfusion with mild bradycardia, soft blood pressure, low EtCO2 and a low pulse ox pleth.
This helps in indicating shunted blood or reduce perfusion to the probe and can be used to help rule in shock states. Most go right to carbon monoxide poisoning, but if I gave you a carboxyhemoglobin in parentheses which we should be monitoring this on all inhalation patients does this change your mind? Also account for the lower than 99-100% SpO2.
Now, carbon monoxide is always great to keep on the front end of your differential list. Don’t forget the enemy lurking in the haze: cyanide.
Cyanide is the devil and it inhibits cellular respiration by blocking the Kreb cycle on the mitochondrial wall. If you can’t generate cellular energy, you lose cellular and tissue function, by losing this the body loses its normal compensatory response and metabolic output.
The reason we see the changes we see are because Marc has cyanide toxicity. He has cyanide that has been absorbed through his capillary bed into his bloodstream and found its way to his mitochondria walls, causing organ dysfunction vasodilation (because the muscles aren’t helping with vascular regulatory tone) blunting his heart rate response and his cerebral perfusion and function.
Not to mention a vast set of other things that aren’t manifesting enough to deemphasize those that are impacting his perfusion and mentation. So, we have ensured he has an airway, that he is breathing, and we also have ensured he has a pulse.
But his perfusion is not as adequate as it should be, so we’ve helped supplement him with some salt water to increase his perfusion.
Now after more findings in our assessment we recognize we need to help his mitochondria by getting that cyanide off of them. In this case we use Hydroxocobalamin to help do that.
Hydroxocobalamin has a cobalt ion that helps chelate (think of it as a chemical crowbar) the cyanide off of the mitochondrial wall. This helps to restore cellular metabolism and function.
And we’ve already added the saline which will help with the clearance of the converted hydroxocobalamin to cyanocobalamin, which is just vitamin B, that will be excreted through his urinary track. As we saw during transport, the functionality of the Hydroxocobalamin started to work as we were getting Marc’s slow return back to baseline.
Marc‘s case is a prime example of a smoke inhalation/toxicity case that wasn’t dispatched as a “fire or smoke” incident. A great example of why we should slow role as we always should our scene size up and patient assessment to ensure we don’t also become victims of the problem .
In Marc‘s case, this was a cold smoke fire and shows us that these inhalation and toxic states aren’t always from large conflagrations. And notice that Kim‘s information to the dispatcher and what was emphasized had nothing to do with the events leading up to.
More from the Author
Friday Night Lights: Shift 15 – Squeaky Peaked Exits
Friday Night Lights: Shift 14 – Wet Whistles and Steak
Friday Night Lights: Shift 13 – Sweet Dehydration
Chris Kroboth has been a career paramedic/firefighter for over 17 years and in EMS for over 23. He has been in prehospital and in-hospital education for the past 18 years. His last assignment before returning to operations was as the EMS training captain in charge of continuing education programs and certification. He is also affiliate faculty with the Virginia Commonwealth University Paramedic Program. He is the U.S. clinical education manager for iSimulate and also facilitates national conference clinical challenges to include EMS World, ENA and NTI.


