
Optimal Prehospital Airway Management Depends on EMS System Efficiency
The authors comment on the prehospital airway debate at the 2020 NAEMSP Annual Meeting.

The authors comment on the prehospital airway debate at the 2020 NAEMSP Annual Meeting.
Many factors go into the equation for deciding between CPAP and BiPAP for a patient.

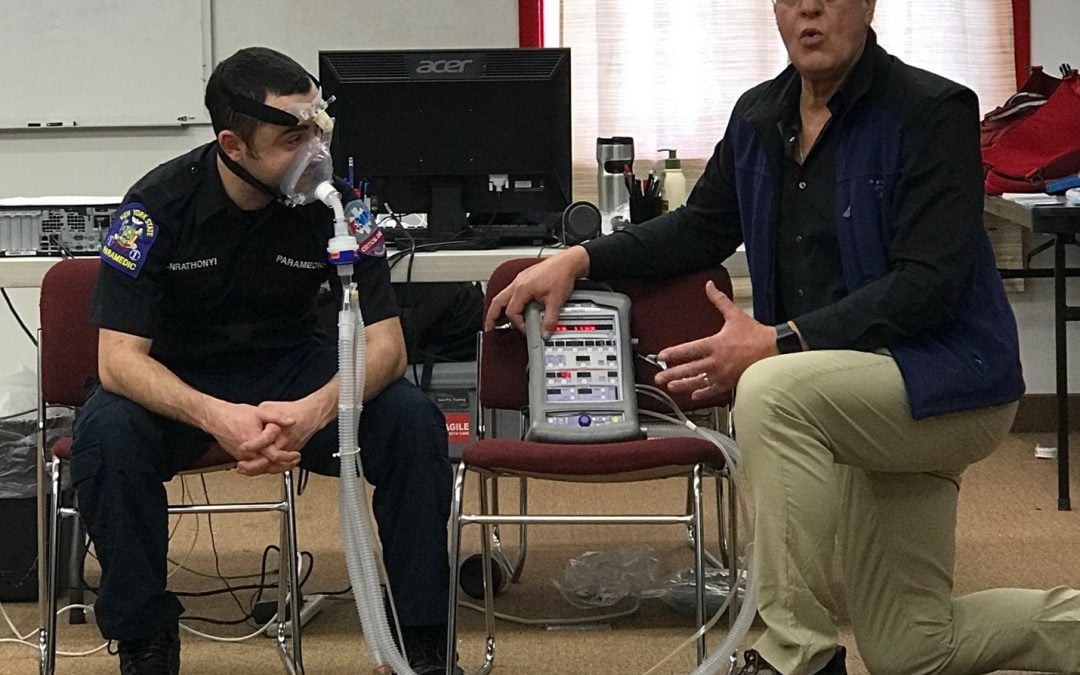
Measuring EtCO2 is the most accurate monitoring tool that paramedics can use in real time to assess the overall status of the patient in the field.

Lifesaving procedures like CPAP pose tremendous risk to patients if miscommunications occur during handoffs. The focus of this article is on reducing these errors.

Understanding the complicated disease of Cystic Fibrosis will help you provide better initial care and assessment.

Use of Positive End Expiratory Pressure should be considered for any patient who requires mechanical ventilation, including those in cardiac arrest.
Recent Comments