
Images provided by the author.
It’s another hot Friday night, where the humidity and the ambient temperature are essentially the same at 98 and 98. You’ve concluded that it’s like working in a crockpot, but there’s nothing better than a cold Poké bowl on these hot, humid nights.
You go with your throwdown tuna and crunchy rice noodles, and your partner goes with salmon, trying to mix it up for the first time. You very much love the taste of the lime on top of the tuna. It’s a fascinating chemistry experiment to look at the tuna change color (a great example of what an acidic environment does to tissue #metabolicacidosis).
You finish up, and before you can ask your partner how theirs was, the CAD chirps; you’re headed to the best ice cream shop in town for a 16-year-old female who syncopized and is having trouble breathing. You gather your trash, put it in the bag on your side, and your partner starts for Tyler’s Creamery.
You banter back and forth and agree that if it’s nothing, you’ll get a chocolate-dipped vanilla swirl with no less than three scoops because you’re not a heathen. Your partner says (with a cheek-to-cheek grin) they’re going for the classic extra-large split.
As you pull up, you find the usual line wrapped around the shop and a young gentleman with the patented ice cream parlor apron and paper hat waving you down from the back door. You both gather the equipment, head around the corner, and find Nikita Williams sitting on the floor with her hands holding her forehead.
You do a quick once-over of the back-end workings of the ice cream shop and then turn back towards Nikita, kneeling and introducing yourself, then asking her, “What happened?” as you try to shake her hand. She doesn’t even notice. You take a quick radial pulse and find it almost absent and fast.
She is slow to get words out. In the background, you hear the manager explaining to your partner that she was bent down, restocking the waffle cone drawer, then stood up, started to wobble, and then fell.
You take what you just heard and try to incorporate it into your conversation with her about how the food and smells here are so good that they must’ve made her pass out. She snickers slightly and says she just feels weak and lightheaded; you work on getting her to elaborate on what she means by weak and what the lightheadedness feels like.
You ask if the room is spinning, if she is spinning, or if it feels like her head is heavy and she can’t pick it up. She picks up her right pointer finger and points to you, gesturing “that one” to the last example you gave.
You ask her if she’s had this before, and she says “once,” slowly and quietly. You ask how long it was, and she says it was last month. You ask her if she’s had any medical problems, takes any medicine, or has any allergies to medicine. She denies all the above.
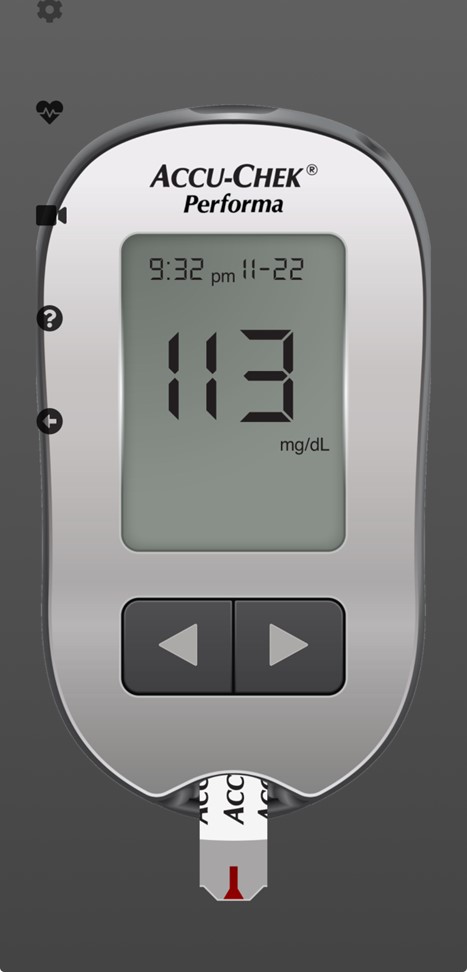
You ask her to squeeze your hands. She grabs weakly on both hands, and you let her know that your partner will be hooking up an EKG, getting a blood pressure pulse ox, and having to poke her finger to get her sugar. You ask her to smile, stick her tongue out, and then pull back on her feet and push down on your hands with her feet.
She does all this symmetrically but with noticeable weakness. Your partner points to the monitor just before getting the blood sugar. You noticed Nikita doesn’t even move with the prick of the lancet. Based on what you see, what are your thoughts? Is anything jumping out of you?
You get back to conversing with Nikita and ask her when she got to work, if she drove here, if she had a typical day, if she had everyday food, etc. She said she drove here and had no other complaints, and the day was usual for her, including school and softball practice. You ask her if there’s anything we should know about.
You whisper to her, “Do you take any street drugs?” “Have you tried anything new?” She adamantly denies both. She said she’s trying to get a college scholarship and has never done drugs nor will ever do drugs. You compliment and commend her for that and tell her to keep up the excellent work.
You ask her if she’s had any falls recently, and she shakes her head no. You ask her if she had her menstrual cycle recently and if there’s any chance she could be pregnant. She picks her head up with a scour, shakes her head no, and says, “There is no way I can be pregnant. But I am definitely on my period!”
What do you think the problem could be in this otherwise healthy, athletic 16-year-old female who passed out while at work after bending down for an extended time?
You ask her if her periods have been regular. She shakes her head no and says the last two have been heavy, with a lot of pain, and lasting almost a week and a half. You ask how many pads she has gone through compared to three or four months ago, and she says about three to four times more, and she had to switch to the “heavy flow” pads.
You ask if she let anybody know about this, and she shakes her head no. She said she thought last month was an anomaly. You ask if you can pull down her eyelids and look at the inside of them. She looks up at you and says, “Sure.” You note they are blanched (hypoperfused) when they should be pink and vasculated. This helps you further confirm the likelihood of low blood volume.
You ask her if it’s OK to take her to the hospital because you’re concerned that her blood volume is low and that her being in the back of an ice cream shop and continuing to work with low volume could cause her to pass out again.
You’re also concerned about her passing out and hitting her head on one of the metal machines. She says she would like that and you ask if there’s a family member that you should contact. She gives you her aunt’s number and says her parents are out of town on a cruise. You call her aunt and tell her what you and Nikita discussed and that you will take her to County General. She agrees and says she will meet you there.
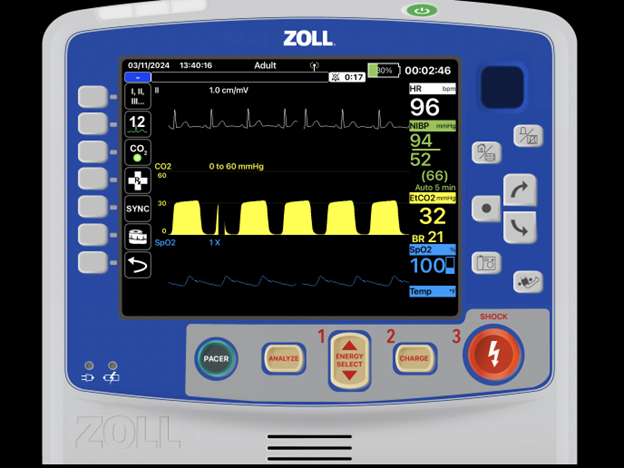
Let’s review the patient’s vitals without capnography and then with.
Would anything jump out at you with the below vitals on an otherwise healthy 16-year-old female.
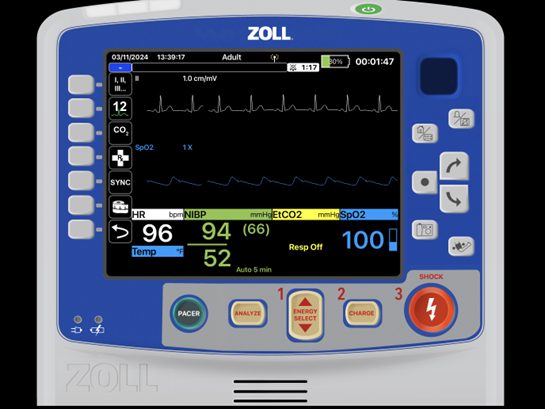
We get conditioned to think, “Oh well, the heart rate is less than 100, so that is normal.” But is it? No! A heart rate should not be at the upper end of normal when the patient is sitting and not stressed. It should be if they just finished a heavy workload. Nikita didn’t just finish a 10-mile run. She was bent over stocking a drawer, passed out, and has been sitting down since.
Also, notice that MAP (link in the references about BP and MAP) is just above 65mmHg. Lastly, look at the amplitude of the pulse ox pleth. It is low, meaning reduced blood flow to where the probe is located, commonly seen in shunted extremities or cold ones. But we aren’t taught to think link this.
Now, with capnography?
What are we seeing? Remember, when the body needs to draw blood back into the thorax, it relies heavily on the negative pressure of breathing. So, we regularly see “trouble breathing” as a symptom of hypoperfusion. Add the end-tidal value, and we can quickly rule in hypoperfusion in Nikita. The history we obtained in our assessment helps solidify this.
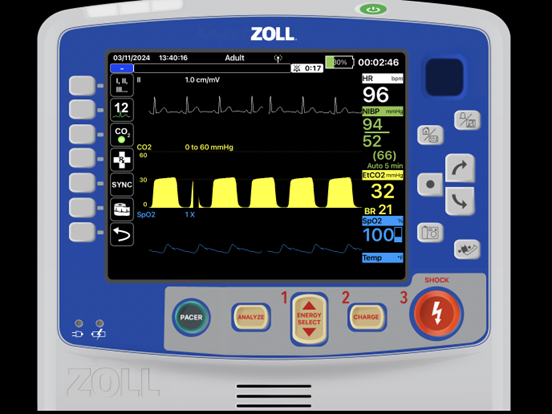
The end-tidal waveform is sound, with D being bigger than C and having a defined B-C and C-D phase with the D-E back to zero.
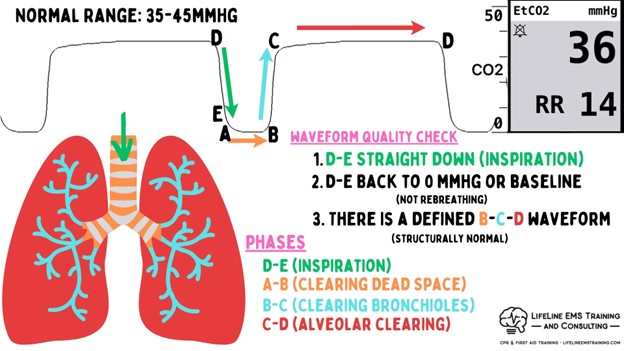
We see the upper-end respiratory rate (especially noticeable when the patient is just sitting) and the lower-than-normal end-tidal. This should drive you early to a perfusion problem. In Nikita’s case, she has above-normal blood loss daily.1
This is a prime example of how end-tidal capnography can help us identify the underlying problem with patients. Capnography gave us the most substantial value.
Reference
1. (n.d.). Heavy menstrual bleeding. Mayo Clinic. Retrieved January 7, 2025, from https://www.mayoclinic.org/diseases-conditions/menorrhagia/symptoms-causes/syc-20352829
Chris Kroboth has been a career paramedic/firefighter for over 17 years and in EMS for over 23. He has been in prehospital and in-hospital education for the past 18 years. His last assignment before returning to operations was as the EMS training captain in charge of continuing education programs and certification. He is also affiliate faculty with the Virginia Commonwealth University Paramedic Program. He is the U.S. clinical education manager for iSimulate and also facilitates national conference clinical challenges to include EMS World, ENA and NTI.


