Images provided by the author.
If your EMS education was anything like mine, you were taught that blood flow returns to the heart under pressure through the venous system and that pressure was positive.
No one ever told you that blood returning to your heart relies heavily on the thorax’s negative pressure, which occurs with every inhalation. In this article, we want to highlight the importance of breathing in returning blood to the heart.
Let’s start with a quick review of the thorax, the “top box of life.”
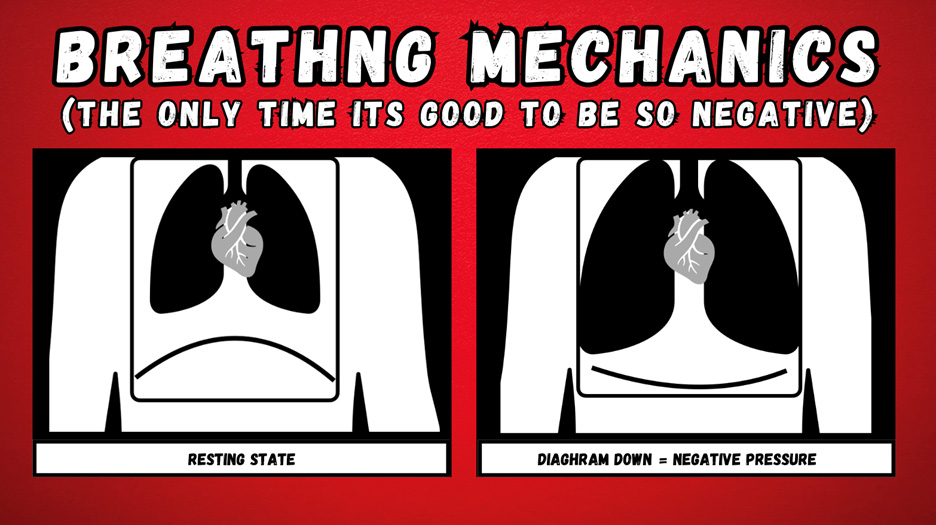
Your thorax is a cavity from below the neck to above the diaphragm spanning inside the armpits to the anterior chest through to the back. Your diaphragm is the main moving piece of the box and is what changes its “container” size.
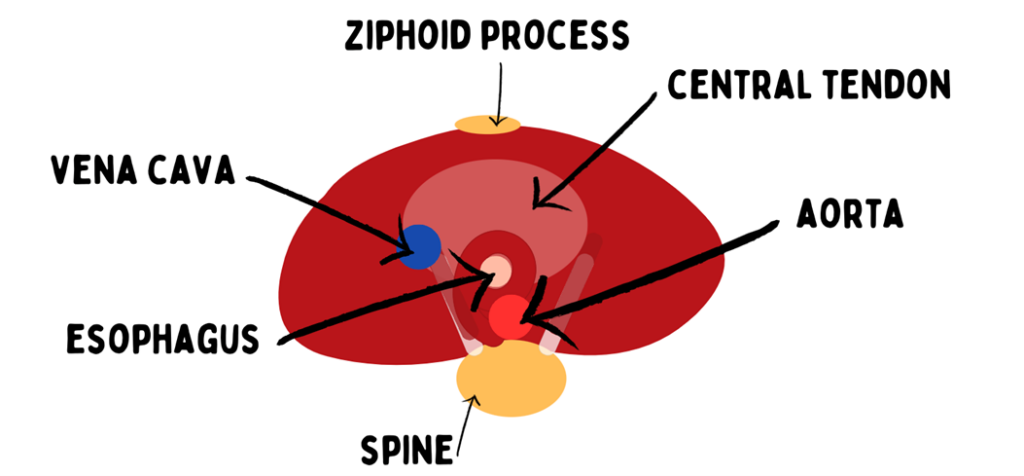
The diaphragm is a muscle made of skeletal muscle and is C-shaped. It goes down to increase the container size and relaxes to decrease it. Within the diaphragm runs your esophagus and great vessels, the vena cava and the aorta.
As we just said, the thoracic container size increases when you take that breath. When you increase the container size and maintain the same volume, the pressure becomes negative (you make a vacuum). You can practice this by taking a soda bottle, cutting off the bottom, and putting a rubber glove on the base and a balloon down the top, as seen in the image below.
When you pull down on the glove, you’re increasing the container size without changing the volume inside, so what does it do to the balloon inside? It expands the balloon because you’ve made a negative pressure environment.

This is your fifth-grade chemistry lesson. You can also see in the image that if that balloon is your vena cava, it swells. The vena cava is a soft, squishy blood vessel compared to the aorta, a dense muscular artery. The vena cava expands in the negative state, drawing more blood back into it.
Now think about your last trauma patient; what was their respiratory rate? It was elevated, wasn’t it? And we were all taught trauma patients raise their respiratory rate; why? Because they need more oxygen in their body, right? What if they need more blood back to the right side of the heart in compensated shock?
Next time you look at your patient, assess their respiratory rate and quality and ask why. Don’t just consider they’re doing it to bring in more oxygen but also to draw more blood back to the heart to ensure good cardiac output.
Circling back to the thorax, the upper box of life and the diaphragms need to go down to increase the container size and make a negative pressure state so that the body can draw in atmospheric air for breathing. What happens to that pressure in the thorax when we put a BVM on the patient’s face and squeeze?
Our respiratory support is all positive pressure support from the 2L nasal cannula and CPAP at 10 cmH2O to the BVM and ventilator. Everything we give is delivered with positive delivery pressure.
So anytime we give oxygen or ventilation support, we will make the thoracic pressure more positive, which means we will also impact venous return to the heart. While that impact may be minimal, it is that effect that all of our ventilatory support has a minimum systolic pressure requirement for treatment, usually around 100 mmHg. When we provide support, we decrease the blood return to the right heart, thus impacting cardiac output.
What are some vulnerable states we find in patients where impacting their thoracic pressure and venous return can make their teetering status tip faster and crash quicker?
I would say the most vulnerable is a ROSC patient. They were just dead; you can’t get more unstable than just dead. Reflect on your last cardiac arrest patient. I hope it was a calm setting with two-minute cycles and systematic care.
But my gut tells me it was not calm, cool, and collected. What was the person with the bag of life (BVM) doing? Were they maintaining an optimal volume at an optimal rate while monitoring the end-tidal?
Sadly, in our business, it’s usually the most novice individual who gets the bag of life; whether pushing on the chest or squeezing the BVM, we tend to put the newer members onto two of the most critical components to resuscitation management.
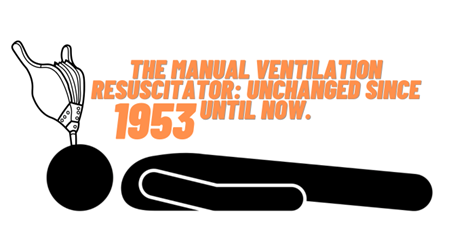
Most agencies have migrated to mechanical compression devices with applications after the third, fourth, or fifth round, but many have not moved to a mechanical ventilator.

New technologies and changes in the BVM include straps to maintain seals when mask/face ventilation is performed. If you’re buying a PEEP valve on your BVM, you need a strap to benefit from the positive end-expiratory pressure while bagging your patient.
The two other vulnerable areas are rate and volume. There’s always a debate about whether or not we should use child BVM to reduce the volume of delivery to our patients.
The counterargument is that there’s not enough volume in the child BVM to create enough driving pressure to deliver adequate volume to patients with restrictive airways or poor positioning.
Regarding the rate, when talking about a manual resuscitator, the rate is at the mercy of the person squeezing the bag. Devices like the VT Select have reduced volume bags still in the adult range, making you less likely to over-inflate.
That device also has a control mechanism that delays the bag’s filling to an interval of around ten breaths per minute. So, they have engineered a stress throttle. When the rate-regulated mode is dialed on, the provider can only ventilate at around ten breaths per minute at the reduced volume.

This is a huge human factor engineering advancement in ventilation management. If you look back, there have not been many, if any, manual resuscitator bag enhancements in the last 60 years, but the ones we’ve highlighted are huge to combat provider stress and mismanagement. It is refreshing to see someone change up tools and devices that are critical in managing the A and B of ABC.
Chris Kroboth has been a career paramedic/firefighter for over 17 years and in EMS for over 23. He has been in prehospital and in-hospital education for the past 18 years. His last assignment before returning to operations was as the EMS training captain in charge of continuing education programs and certification. He is also affiliate faculty with the Virginia Commonwealth University Paramedic Program. He is the U.S. clinical education manager for iSimulate and also facilitates national conference clinical challenges to include EMS World, ENA and NTI.


