
On the go? Listen to the article below!
PEEP Use in BVM Management
Before you start reading this article, I want you to sit back, relax, and take a deep breath. How refreshing was that? That was a nice 21.3% (ish) atmospheric oxygen breath that your body just enjoyed. Please keep that thought in the back of your mind for a minute. We will revisit that. We will spend a moment on PEEP, not the delicious and iconic Easter marshmallow treats that have become a yearly staple for many, but Peak End Expiratory Pressure. For this bit of time we have together, we will focus on why PEEP should be your go-to for desaturating patients or patients needing their SpO2 to rise.
Think back to your initial training; what was the answer for a low SpO2 in patients? You should say something like 15LPM non-rebreather for the patient, bystander, dog, next-door neighbor, and any other biological being existing in the same zip code, to include the person evaluating the scenario. We were always taught that low SpO2 = crap tons of oxygen STAT (speaking of STAT, it’s O2 sats as in saturation, not STATS). Sadly, we were all taught and evaluated incorrectly. When a person lacks Oxygen (saturation), hypersaturating the atmosphere they are breathing doesn’t necessarily mean that extra oxygen actually binds to the RBC’s hemoglobin. Since we all usually live comfortably off of that same delicious 21.3% you enjoyed earlier, it’s likely something else causing the poor exchange and circulation of oxygenation.
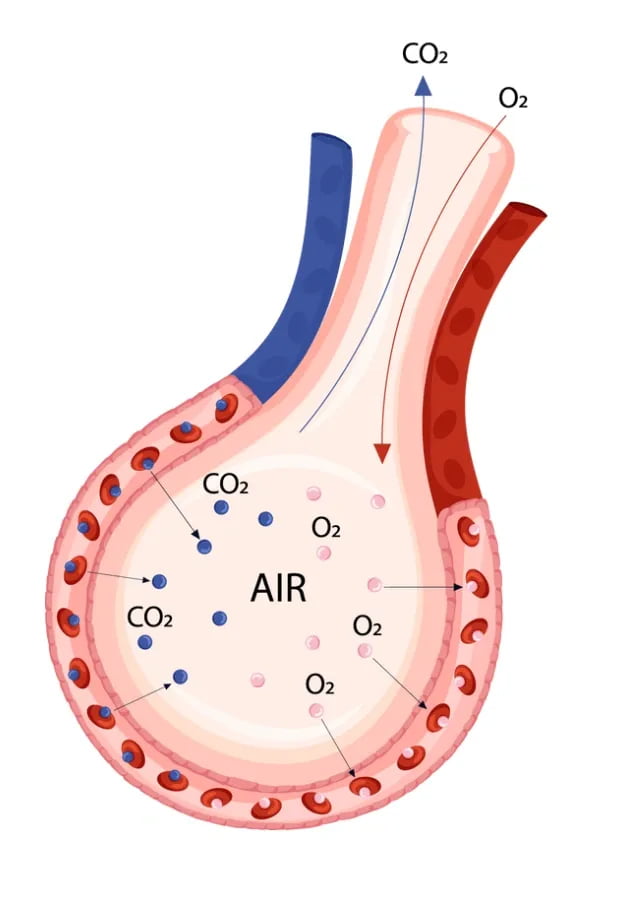
Going back to the basics of airway anatomy, we all remember the alveoli is the air sac with a single-cell thick wall that expands on inspiration and is wrapped in capillaries that allow for gas exchange (diffusion).
For simplification, let’s call these alveoli balloons. If you were at a party and noticed the balloons were starting to sag and drift down, what would you do to help bring them back to life? You’d blow them up, right? That would increase the gas in the container, filling them up, increasing their surface area, and making them festive and functional again. Well, what if that thin balloon wall allowed for gas exchange? What if that wall surface area is where Oxygen went over into the capillaries wrapped around it (by the way, the capillaries are a single cell thick too, so when the balloon is stretched, they do too, making diffusion easier)?
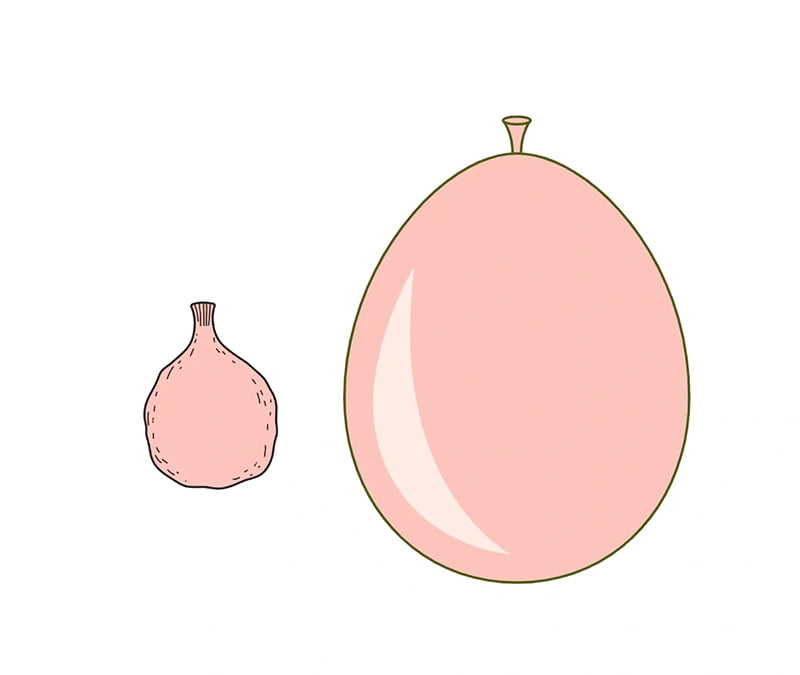
This is why PEEP should be your go-to when you have a patient who is not oxygenating. It helps expand the oxygen exchange capacity by increasing the surface area where gas can diffuse. Or, for those of you not (yet) fluent in Nerd, it blows up your alveolar “balloons” to allow more space for the oxygen to crossover into the bloodstream. This is also why in pulmonary edema, PEEP is of huge benefit. It expands the alveoli and increases the area not in contact with the edema or fluid. The bigger the balloon, the more space for gas exchange that isn’t restricted by the fluid in the balloon. Oxygen can’t diffuse through a liquid, but CO2 can. That is why you can use capnography effectively with pulmonary edema/drowning patients, as the CO2 diffuses through the liquid easily.
What does a PEEP valve do? A PEEP valve prevents complete emptying of the alveoli by providing back pressure on the exhalation port. You pick the pressure you want based on how much ballooning you need to enhance oxygenation.

In the case of the party balloon, the PEEP valve is the fingers you use to pinch the end while you take another deep breath to continue blowing it up. They are preventing the complete emptying of the balloon.

However, this doesn’t come without adverse effects. The more we balloon the alveoli, the more we increase thoracic volume (air in the container that is their chest); the more we increase thoracic volume, the more we push and pinch the vena cava. The end result is decreased venous return as we escalate our level of PEEP.
Now think about when we are bagging patients lying supine. What is the weight of the thorax doing to the chest cavity and to our ability to effectively ventilate the patient against that resistance? This is another place PEEP can help. PEEP helps maintain alveolar inflation against that increased weight and resistance.
OK, so I think it’s safe to assume that you’re now sold on the benefits of PEEP. If it’s this important, we should utilize it with our BVMs just as much as with our CPAP circuits. So what gives? When we squeeze our positive pressure breath into the patient, the goal is to provide enough volume (and pressure) to inflate the alveoli and establish adequate gas exchange. But do we do this well? Do we establish a good seal? Do we maintain constant volume and pressure? I’d say we can all agree we don’t. In fact, in most instances, the person holding the bag of life (BVM) is the team’s newest member, and they struggle to balance appropriate seal, rate, and volume, all while not letting their adrenaline overdrive their ventilatory support. What can we do to fix this?
We haven’t changed the BVM since its inception in 1953; we have “tried” to train best practice ventilation through all levels of healthcare and with our every 2-year alphabet soup courses. But we still provide poor seals and regularly over-ventilate by rate and volume. One quick fix with a big payoff is using a strap around the BVM mask to help ensure a good seal. With a good seal and a PEEP valve, we keep the alveolar balloons inflated between breaths. While the gold standard for achieving a good seal is a two-person approach– one to hold the mask and one to squeeze the bag, we all know manpower is at a premium on scene. This is the part where I let you know that I receive no kickbacks for Pulmodyne for this recommendation. That said, Pulmodyne has a great and cheap silicone strap that can easily be applied for a great one-handed seal and rolled away if the patient vomits.


This allows for an effective seal, one-person BVM management, and PEEP valve function. Now with your BVM mask, you can maintain a seal even without your hands. By applying a strap and ensuring a seal, you can maximize the oxygen exchange surface area and overcome the resistance from the weight of the patient’s thorax.
Or send them here for more BVM tips.
Reference
1. Ni SA, Carpenter RS, Walker JR 3rd, Holley J, Brady MF. Emergency Medical Services Responder Manual Ventilation Performance. Prehosp Emerg Care. 2022 Jun 9:1-5. doi: 10.1080/10903127.2022.2066234. Epub ahead of print. PMID: 35442149.
Chris Kroboth has been a career paramedic/firefighter for over 17 years and in EMS for over 23. He has been in prehospital and in-hospital education for the past 18 years. His last assignment before returning to operations was as the EMS training captain in charge of continuing education programs and certification. He is also affiliate faculty with the Virginia Commonwealth University Paramedic Program. He is the U.S. clinical education manager for iSimulate and also facilitates national conference clinical challenges to include EMS World, ENA and NTI.


