Images provided by the author.
It’s the last Friday of the month, which means nothing but the summer concert series on the lawn. Your partner is excited to hear the Dave Matthew’s cover band play “Two Step.” You both opt to grab a quick bite at Gino’s and head over to the park so you can enjoy some live music.
You park outside the main area, hop out of the rig, and head to the lawn with your world-renowned cheesesteak. You both sit down behind one of the Park and Rec ATVs, unwrap your steak and cheese, and enjoy the first (actually warm) bite. You were convinced to try it with banana peppers for the first time in history, and it doesn’t disappoint. It is beyond delicious, and you look to your partner, thanking them for forcing you with peer pressure to try it with the peppers. Your partner begins to reply with a “told you so,” and your radio chirps, sending you to a 58-year-old male with trouble breathing.
You snag one last bite, knowing your banana pepper cheesesteak experience will be cold and nowhere near delicious as it is fresh. You gather things up and head back to the rig. You hop in and mark en route. The house is about three miles away, and traffic is light because everyone is downtown hanging out.
You pull up to a rambler on a slight hill with a pristine checkered pattern cut into the lawn, and you see a female at the door waving you over. Your partner puts the rig in park, and you both gather your equipment and head up to the house. The patient’s spouse says, “he’s over there on the couch; he can’t breathe.”
Around the corner, you find a gentleman supine on the couch with his eyes closed, breathing fast at what looks to be a normal depth. You ask the spouse for the patient’s name, and she says Buddy Clarke. You turn back to the patient, kneel down, and go to shake his hand while asking him, “Mr. Clarke, how are you feeling?”
He mumbles incoherent sounds. You shift from shaking his hand to checking his radial and carotid pulse. You note by now, that his respiratory rate is about one breath every one and a half to two seconds, and he feels clammy but warm. You look at your partner to get him hooked up and grab a blood sugar while you step back and ask the spouse what Mr. Clarke’s medical problems are, what allergies to meds he has, and what medications he takes.
You also inquire about what’s been happening for the last few days. She tells you he has a history of high blood pressure, has no medication allergies, and takes HCTZ. He hasn’t had any recent travel. He had a tooth implant placed two weeks ago but has been tolerating well and doing fine since.
You ask if anybody has been sick at home, and she denies it. You ask, “What does he do for work, and what is his free time?” You notice she looks very stressed, but she’s trying to process the question, and you try to lighten her up.
“Does he do anything like MMA fighting, skydiving sword fighting?” She looks up at you and smiles slightly, denying all of those. She says he loves to fish, and his occupation is machine part sales. You try to gather if he has traveled recently by car, air, train, etc. She denies all the above. Your partner gives you a half nod to take a peek at the monitor and you find the following:

What do you see here that jumps out to you, and what is a concern?
You want to listen to Mr. Clark’s lungs and do a couple more tests, then auscultate the lungs and hear the following.
During your continued assessment, Mr. Clarke has clammy extremities and a warm core, no pitting edema, no trauma and no mottling to the skin. He has steady, fast breathing and mumbles when you ask questions. You listen to the side of his throat and hear clear air movement.
You ask when he last ate, and his wife says he hasn’t had much appetite, but she got him a hard-boiled egg and avocado on toast last night. Does he usually eat well? She looks over to Mr. Clarke, gesturing with her hand up and down. He didn’t get that physique by fasting (He’s about 230lbs and 5-foot 7-inches tall).
What are your differentials so far? What are you most concerned about?
You ask if he’s had any recent gains or loss in weight, and she denies both. Your partner grabs a temperature that shows the following:
You ask her how long he has been lying on the couch and what he was doing before. She says she walked downstairs this morning and found him this way. You ask what time they went to bed last night. She says about 10 p.m. Nothing was abnormal about their day yesterday except that he was tired and didn’t want to go on their usual evening walk.
Your partner shows you the below:
So, what is happening? Looking at Mr. Clark’s vitals and his history, sepsis should be high on your differential list. It is not uncommon for people to call or present with the symptom of “trouble breathing” for a person who is septic or in septic shock. Their respiratory rate is up, and often, their depth is up while they are in a state of reduced perfusion.
Let’s examine Mr. Clark’s vital signs and conditions and match them to his history. We can quickly put sepsis high on our differential list. SIRS criteria does a good job of helping us correlate the why to the what with physiologic changes in states of stress like sepsis.
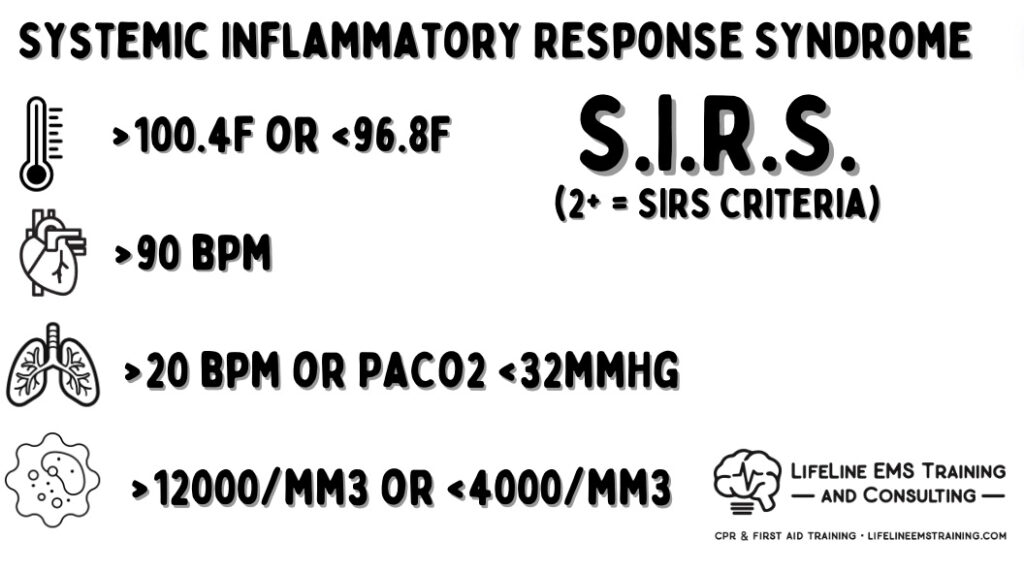
When a person has an infection in their body, their body starts to mount an attack. Part of this attack is generating a fever to make sub-optimal conditions for bacterial proliferation, and this includes bacterial, fungal, protozoa, and other biological and non-viral infections.
Fevers are part of the attack, hence why viral infections traditionally have low-grade fevers and live infections have higher fevers. But don’t take that to heart because patients could have taken antipyretic medication like Tylenol, which dropped their temperature before your arrival.
How do you make a fever? You have to have the metabolism to generate heat. Think about shivering in winter; your body triggers muscle activity to generate heat. Same for infection, but it is the spike in metabolism that drives the temperature up.
So, what is required for this cellular metabolism? Cells need sugar and oxygen for metabolism. How do they get the oxygen? You increase your respiratory rate. So, patients with infection will commonly have higher than normal respiratory rates to help drive more oxygen and support perfusion and carbon dioxide offloading.
How do you generate sugar? Your body releases cortisol, the stress hormone, which helps break down glycogen stores in the back of the liver to make bioavailable sugar for cellular metabolism. Street tip, when you have a patient who has an elevated blood sugar, doesn’t have a history of diabetes, and hasn’t recently eaten a large meal, you should have a high suspicion that they are experiencing a stress response.
As the body fights the infection, the metabolism and cellular activity continue to ramp up. Your body has to eliminate the byproducts of this. As the cellular activity increases and the perfusion starts to decrease, the cellular respiration changes from aerobic to anaerobic, and the volume of the patient starts to decrease from increased urination and breathing.
As that volume decreases the ability to offload the byproducts and continue high rates of metabolism goes down as well. For the metabolism, we bank on the free-floating bicarbonate from the kidneys to react with the hydrogen ions from cellular metabolism to neutralize and break down into H2O and CO2 (pee and breathe).
As your body continues to fight the high metabolic state, the kidneys can only support this bicarbonate production for so long, as bicarbonate production goes down then hydrogen ion acidosis starts to go up. Imagine running on a treadmill for three days, you’d be in a severe lactic acidosis, and your body would not be able to maintain a solid compensatory ability.
The easy and quick compensatory mechanism of the body to help with metabolic acidosis is breathing fast and deep. The body can blow off CO2 (a weak acid) to try to help and neutralize this.
So, with metabolic acidosis the body initially tries to compensate with the respiratory track, as our acidosis continues to worsen in the body, we take our organ function out of its optimal temperature and pH range which means cellular function starts to go down, this is where sepsis progresses into septic shock.
Their blood vessels also become irritated and release nitric oxide causing vasodilation. When we become acidotic the heart becomes floppy meaning the heart’s contractility is down. If we go back to the formula:
A person in septic shock has reduced volume and reduced contract or stroke so the only other part of that formula that can compensate is the heart rate. This is why it is not uncommon to see septic shock patients with heart rates in the 120s and 130s because that is the only portion of that formula that can still effectively regulate.
Looking at Mr. Clarke and his vital signs, how do we want to treat him? We recognize he has the septic shock bundle, tachycardia, and poor perfusion verified by low end-tidal and low MAP. (Our target is 65mmHg). He also has a fever and elevated sugar. In the prehospital community, there are three priorities for sepsis. We need to do a good assessment, sepsis recognition with alert, and perfusion restoration. We want to ensure there is good end-organ perfusion and renal cleansing before we start dumping a bunch of other medications into the patient.
Going back to the blood vessels releasing nitric oxide in the acidotic state which creates the massive vasodilation, so along with fluid resuscitation, we may have to administer an alpha agonist like nor-adrenaline to help with the vascular lockdown reducing the container size.
We start two IVs on Mr. Clarke and start him on a 30 ML/kg bolus of saline and watch for physiologic change. In his case, this would be a reduction in the heart rate and elevation of the MAP and EtCO2. Side note, if the patient starts to urinate, that is a great sign! Although it requires cleanup, it is a huge win for the patient’s renal perfusion and byproduct release.

Here are some takeaways from this case: While the symptom or dispatch was trouble breathing, it isn’t always a problem with the respiratory system itself. It may be perceived by family or the patient’s caregiver that the person cannot breathe when they’re using their airway and their respiratory system to help compensate for an underlying condition or poor perfusion. Don’t forget venous return relies heavily on the negative pressure in the thorax by breathing to draw blood back to the heart.
Chris Kroboth has been a career paramedic/firefighter for over 17 years and in EMS for over 23. He has been in prehospital and in-hospital education for the past 18 years. His last assignment before returning to operations was as the EMS training captain in charge of continuing education programs and certification. He is also affiliate faculty with the Virginia Commonwealth University Paramedic Program. He is the U.S. clinical education manager for iSimulate and also facilitates national conference clinical challenges to include EMS World, ENA and NTI.


