
All images provided by the author.
You’ve known your partner for ten years now and never thought you’d hear the words “AÇAÍ” or “KALE” come out of their mouth. You sit back and glance over at them with a “Who are you and what did you do with Kevin?” look. You maintain that look as you enter the new smoothie/bowl shop. Five minutes later, you two walk out with a protein AÇAÍ bowl and “warrior strawberry smoothie” and hop in the rig. You will never admit that both taste delicious, and luckily for you, the CAD chirps sending you to an SOB call about two miles away. You take one more sip and respond over.
As you pull up, you notice a fit tall gentleman pacing back and forth. He looks anxious. You hop out of the rig and introduce yourself. He says his name is Jon Swabe and he was carrying the trash down the stairs at his apartment and missed the last step and jolted down on his left leg. He feels anxious, like he can’t catch his breath.
You ask if you can get him in your rig, and he agrees. He sits down and upright on the cot and is very jittery. You get a history on him and find out he is healthy with no problems or history.
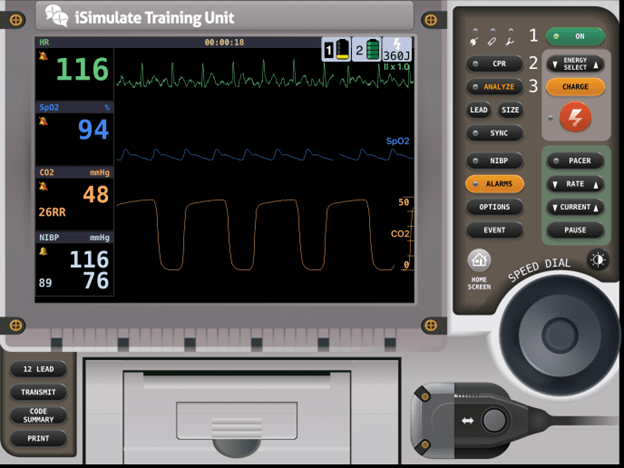
Your partner hooks him up to the monitor and find the following:
What are your primary thoughts?
What is your main concern with the vital signs and waveforms?
You continue your assessment and recognize Jon is taking fast but shallow breaths. He says in two-word sentences, “ I feel………very light……..headed.” He gets more anxious and keeps adjusting himself maintain sitting up straight.
What could be wrong?
You try to listen to lung sounds, but he isn’t taking very deep breaths, so hearing good sounds on either side in all fields is hard.
You tell your partner to hop up front and head to University Hospital. You call in the report, and no other changes happen with Jon en route, and you transfer him to bed 22.
What is Jon’s issue?
Jon has a pneumothorax. He falls into the category of tall, skinny individuals who are prone to pneumothoraces with rapid accelerating or decelerating trauma, mainly occurring when in a vertical plane. Tripping off a curb, over a dog, down a step, jumping down, etc.
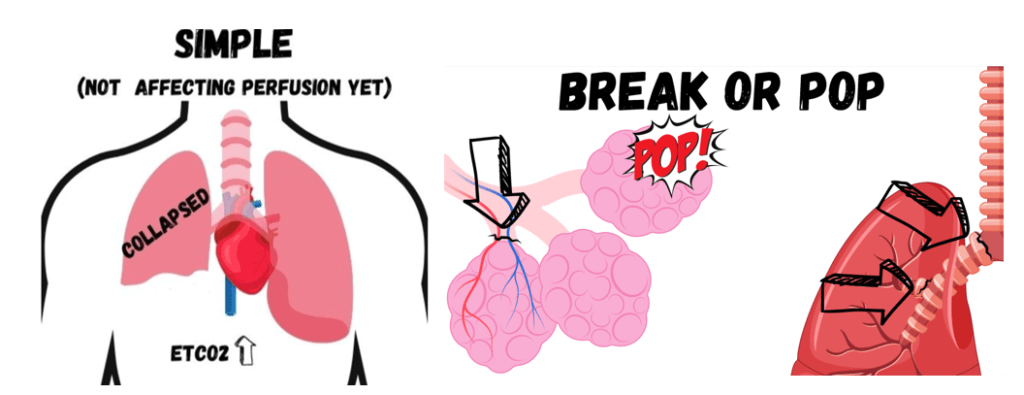
There is a common link to connective tissue disorders like Marfan’s, which cause changes in the fibrous connective tissue. The taller the person, the higher the center of gravity and potential energy. However, it is not only the tall who are affected.
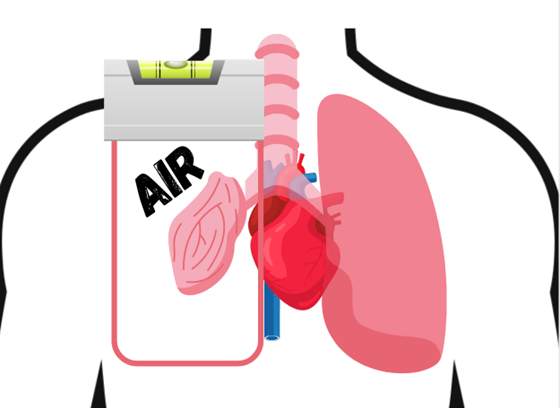
With a pneumothorax (not in tension), the patient loses their ventilatory ability by a reduction in one or a portion of the lung capacity. This causes an elevation in End Tidal CO2 by the reduced ability to ventilate out. The patient also will breathe shallow to not increase the volume in the thorax. You’ll also need an increased rate to help maintain an adequate minute volume (MV= RRxTV). Their heart rate will go up, and also their anxiety from the stress response and catecholamine dump. You may see them continually adjusting to try to stay upright to get the level effect.
The test question answer is “silent lung sounds on one side,” which is a later sign. The air rushing through the airways resonates on the walls, making lung sounds. If the air volume is reduced, the sound will also be reduced. The challenge in a pneumothorax patient, even early is breathing fast and shallow, which in itself reduces the sounds. On top of the fact that good lung sounds are almost impossible to hear in the back of an ambulance or aircraft. Using EtCO2 to help drive your differentials and patient status is a solid choice.
Chris Kroboth has been a career paramedic/firefighter for over 17 years and in EMS for over 23. He has been in prehospital and in-hospital education for the past 18 years. His last assignment before returning to operations was as the EMS training captain in charge of continuing education programs and certification. He is also affiliate faculty with the Virginia Commonwealth University Paramedic Program. He is the U.S. clinical education manager for iSimulate and also facilitates national conference clinical challenges to include EMS World, ENA and NTI.


