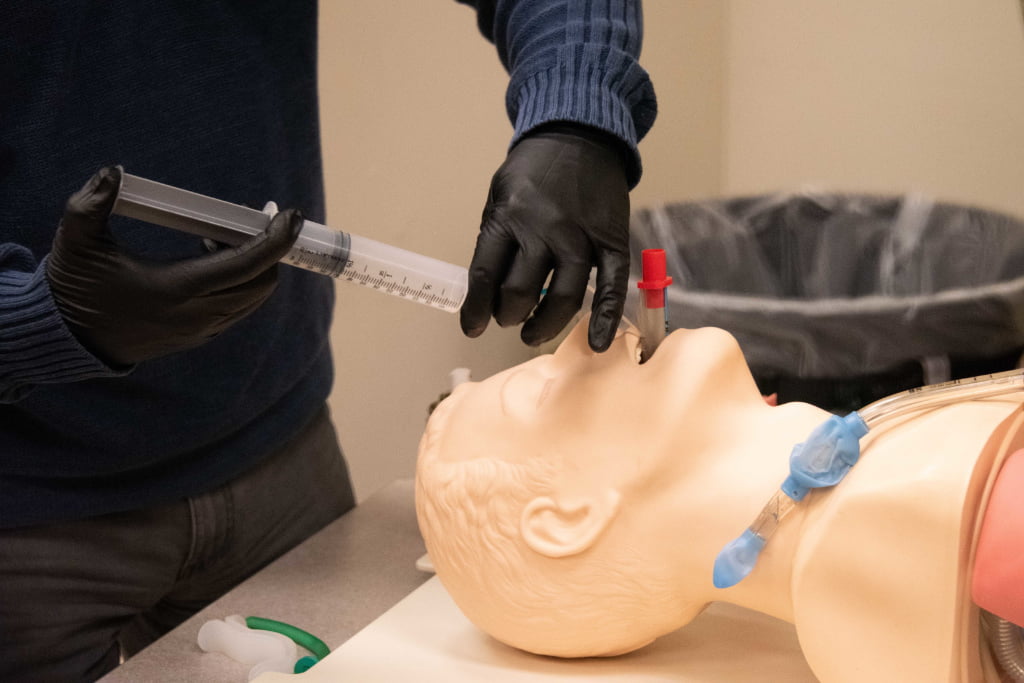
Photo/Greg Mason
“Rescue 43, Ladder 43, Battalion 43 respond reference unresponsive patient at 1419 Paradise Drive.” You arrive on scene to find a 65-year-old male lying on the ground in his living room after he was found unconscious by his wife. The patient does have a palpable carotid pulse, but appears to have vomit and secretions around his mouth. His breathing is slow, shallow and ineffective. While you are formulating a list of differential diagnoses and a clinical plan, your first priority is to secure a patent airway and ensure adequate ventilation and oxygenation. What should your next steps be?
One of the most important aspects to successful airway management is utilizing a team-based, systematic approach, such as utilizing the 6 P’s to successful intubation: preparation: preoxygenation, pretreatment, paralysis and induction, placement with proof and postintubation management.
Preparation: Being prepared to effectively manage an airway by preforming a rapid sequence induction is multifactorial and requires a high degree of knowledge, experience and coordination amongst all parties involved. Preparation is arguably the most important component of airway management. This means that the clinician must have all their equipment ready, the patient is positioned appropriately, and their medications are drawn up and dosages and volumes are verified by two providers. The clinician must also be able to anticipate a difficult airway scenario and understand how to respond to any adverse side effects of intubation that may present before, during, or after the procedure.
Ensuring equipment is ready is of utmost importance during this step. Selecting endotracheal tube size is one of the initial decisions providers will face. Tube size is based on the internal diameter of the endotracheal tube, and sizes typically range from 2.5 mm to 9.0 mm. Tube size selection is often based on individual provider experience and the general circumstances surrounding the intubation. For example, a patient with growths in their airway superior to their glottic opening or edema of their airway due to an inhalation injury may require a smaller tube size. Along the same train of thought, a short petite female patient may require a smaller tube size, whereas a large stockier male may be able to accommodate a larger diameter endotracheal tube size. In general, an adult male will tolerate an 8.0 to 9.0 mm tube, and an adult female will tolerate a 7.0 to 8.0 mm tube. Pediatric tube sizes can be obtained from a length-based resuscitation tape or the following formula: (Age / 4) + 4.
Laryngoscope blade size and style are additional considerations providers must make. The two primary blade styles include Macintosh blades and Miller blades. The Macintosh blade is a curved style blade that is directed into the vallecula to indirectly displace the epiglottis to allow for entry of the endotracheal tube. The miller blade is a straight blade that is used to directly displace the epiglottis to facilitate passage of the endotracheal tube. Sizing for adults is again often based on experience and individual patient anatomy. Most adults can be intubated with a Mac 3 or Miller 3, but longer or shorter blades may be required for patients with shallower or deeper airway anatomy. Length based resuscitation tapes are again a great resource for determining equipment used in pediatric intubations.
Having difficult airway equipment within hands reach is also essential. This includes a bougie, a supraglottic airway device, and equipment to perform a surgical or needle cricothyrotomy. This would also be the time for the provider to ensure that vascular access has been obtained in the form of an intravenous or intraosseous line and that the point of access is patent. In addition to the primary access point, the preference for this patient would be two points of vascular access.
Preparation of medication is an essential component of this step. This includes selecting the appropriate induction and neuromuscular blocking agents at the appropriate dosage and labeling syringes as necessary. Proper selection will be discussed in greater length below. Adequate preparation also includes ensuring a provider crosscheck occurs amongst at least two qualified clinicians of the intubation team to ensure that the appropriate medications and doses are being administered. This also ensures that the person responsible for managing the airway is ready for induction and paralysis prior to administration.
Some agencies have moved towards the use of video laryngoscopy as their standard for laryngoscopy. If available, providers should maximize their proficiency with the skill of video laryngoscopy. Hypes (2016) reported an 80.4% first pass success with the employment of a video laryngoscope device compared to a 65.4% first pass success rate with a direct laryngoscopy approach.1 Additionally, Wayne (2009) reported the average time to successful intubation being 21 seconds when using a video laryngoscope versus 42 seconds with the use of a direct laryngoscope approach.2
Numerous methods exist for anticipating the existence of a difficult airway. This is an essential aspect of airway management, as predicting a challenging airway is an important component to assist in determining the most optimal approach to airway securement.3 The LEMON (Look, evaluate, Mallampati score, obstruction, and neck mobility) mnemonic, which includes the 3-3-2 rule and the Mallampati score, is one well-known method of evaluating for the potential presence of a difficult airway.
The facilitation of intubation can bring forth several compounding adverse outcomes, such as aspiration, apnea, hypoxia and peri-intubation cardiac arrest.7 These events can be precipitated by the consequences associated with the initiation of positive pressure ventilation or the sympathetic nervous system suppression caused by induction agents, thus providers must be prepared to manage these situations.
Another significant component of preparation for intubation includes adequate positioning. One of the most common reasons that clinicians fail to pass the endotracheal on their first pass attempt is due to the lack of attention paid to the importance of appropriate airway positioning. The goal of this stage of airway management involves optimizing the view of the glottic opening during laryngoscopy. Newer EMS professionals are taught in their education programs that the patient should be supine with the patient’s head in a neutral in-line “sniffing position” to help optimize the view of the airway.8
This sniffing position has been shown to show no statistically significant advantage over simply extending the head when utilizing a Macintosh 3 blade.9 Schmitz (2021) reported that “the sniffing position improved glottic exposure in 18% of patients and worsened it in 11%, in comparison with simple head extension in patients intubated in the operating room.”10 The addition of a pad under the occipital region of the head while the patient’s head is in a sniffing position is another method of opening the airway and reducing the angle of the trachea to allow for the passage of the endotracheal tube.
An Emergency Guide to Mechanical Ventilation
A newer patient positioning technique termed “ramping” a patient includes placing a pillow or pad under the shoulders of a patient to facilitate a more “heads up” position to attempt intubation with. This technique helps the clinician to overcome body habitus in obese patients that may further complicate an already difficult intubation.11 In addition to the anatomic differences posed by an overweight patient, these patients present with a decreased functional residual capacity and total lung capacity due to the additional weight exerted on the patient’s chest and abdomen.10 This results in difficulty preoxygenating and denitrogenating these patients, thus the ramp position can also help to facilitate preoxygenation. Khandelwal et al. (2016) reported a decreased risk of aspiration when a patient is in the ramp position and found a decrease in inadvertent esophageal intubation.12 Turner JS et al. (2017) also found that for each increase in head of bed by 5 degrees, the odds of first pass success is increased by 11%.13
Preoxygenation: The peri-intubation period in the prehospital setting is arguably one of the most dangerous times a patient undergoes during the acute phase of their illness. Rates of hypoxia and hypotension reach 20 to 30% in the emergency department for patients undergoing emergent intubation, which would lead one to assume that prehospital statistics are at that same rate or even greater.14 Long et al. (2020) reports that the preoxygenation phase of the airway management algorithm is a vital step preformed prior to intubation that can help to minimize any adverse outcomes associated with complications of the peri-intubation period.15
The main goal of the preoxygenation phase is to extend the patient’s safe apnea time, which is the duration of time that lasts from the time the patient stops breathing until the arterial oxygen concentration drops to an unsafe level – which is typically considered 88% to 90%.16 The primary mechanism that is utilized to extend the safe apnea time is denitrogenation of the lungs, which is done by replacing the nitrogen that exists in the lungs with pure oxygen in all of the oxygen carrying compartments of the body, such as the lungs which serve as the primary oxygen reservoir of the body during apnea. Under optimal conditions, while a person is breathing room air, which is comprised of 21% oxygen and 79% nitrogen, approximately 450 mL of oxygen is present in the lungs of the average healthy adult.16
By preforming effective preoxygenation with 100% FiO2 through a nonrebreather, CPAP device, or ventilating with a bag valve mask, nitrogen is washed out and the oxygen reservoir of the lungs is increased to approximately 3,000 mL of O2. This increases the safe apnea time of an appropriately preoxygenated patient to eight minutes, compared to about one minute in an individual that is breathing room air. It is important to note that critically ill patients may experience critical desaturation at faster rates due to their condition despite focused attempts at preoxygenation.
Another aspect of preoxygenation is the employment of passive oxygenation using a nasal cannula. A nasal cannula can be used throughout the preoxygenation period in addition to the primary oxygen delivery device and left in place throughout the intubation attempt to continue to provide passive oxygenation to the patient. By utilizing a nasal cannula with an oxygen flow rate of 15 lpm, patients can continue to have nearly 100% oxygen supplied to their alveoli during apneic periods, which continues to work to increase the time to desaturation of apneic patients. This method has been shown in multiple randomized control trials to have increased time to desaturation during intubation by nearly two to four minutes of apnea.17 It is important to recognize that this passive oxygenation during intubation is not ventilation, so the development of hypercarbia is possible, and can lead to cardiovascular collapse if not monitored and treated when identified.16
Nickson (2020) shares the following method from conducting preoxygenation:16
- May administer ketamine to facilitate preoxygenation: Administration of ketamine maintains an intact respiratory drive to allow for adequate preoxygenation. IV ketamine administration should be over a 2-5 minute slow IV push. The administering provider must use caution when delivering this medication, as rapid medication administration may cause a brief period of apnea. This is a part of the delayed sequence intubation procedure that may be used to improve preoxygenation.
- Position the patient ‘heads up’ at 30 degrees, with ear above the sternal notch: Positioning appropriately increases functional residual capacity of lungs and utilizes the full capacity of the lungs to be used as a reservoir for oxygen.
- Ensure airway patency: Consider the use of oral and nasal airway adjuncts.
- Place nasal cannula (at 15 L/min oxygen) for passive oxygenation
- Select preoxygenation device based on the patient’s SpO2:
- if SpO2 >95% use:
- bag-valve-mask (BVM) with PEEP valve and a good seal at 15+ L/min O2 or more, or
- non-rebreather (NRB) mask and a good seal at 15 L/min O2 or more
- if SpO2 <95%:
- BVM with PEEP valve and a good seal at 15+ L/min O2 or more
- if SpO2 >95% use:
- If adequate respiratory drive, preoxygenate by:
- At least 3 minutes of tidal ventilations, or
- 8 breaths with full inspiration/expiration to achieve vital capacity in <60 seconds (requires patient cooperation)
- If inadequate respiratory drive, preoxygenate by:
- positive pressure ventilation with PEEP valve (assisted breaths with BVM or NIV)
Pretreatment
The mantra of “resuscitate before you intubate” comes to mind when considering factors involved in pretreatment. This verbiage refers to the use of blood or fluid administration along with the use of push dose vasopressors and vasopressor infusion initiation to stabilize a patient’s condition prior to intubation. Three common denominators have been identified that have been attributed to clinical decline in hemodynamically unstable patients. This includes peri-intubation hypoxia, peri-intubation hypotension, and a pre-intubation shock index greater than 0.9. Peri-intubation hypoxia has been extensively addressed in the preoxygenation section of this literature.
In cases of hypotension and elevated shock index, whether it be due to traumatic or medically related hypovolemia/hypotension, there are numerous interventions that are well-within the scope of practice of prehospital care providers. In cases of traumatic hypovolemia, blood products are the first choice in response to hypovolemic shock and an elevated shock index. An additional adjunct that can be utilized by paramedics and critical care transport professionals in cases of traumatic or medical etiologies is the employment of push-dose vasopressors. These agents have been used for years in the anesthesia setting but have more recently become a valuable tool for emergency department and transport professionals. They can be used to increase cardiac output and prevent peri-intubation cardiovascular collapse during intubation. These can be utilized as adjuncts to prevent and/or treat cases of transient hypotension caused by the suppression of sympathetic tone throughout the body during intubation. One of the most recognized pitfalls to the use of push dose vasopressors is the risk for dosing errors, which can be ten to one hundred-fold the dosing error.
Respiratory Syncytial Virus: It’s the Season
In a 2019 study, Cole et al. (2019) focused on emergency department push dose pressor usage and demonstrated a 19% dosing error when compared to the intended dose.18 Fortunately for prehospital care providers, Nawrocki et al. (2019) found that of 100 doses of push dose epinephrine administered over a two-year period, 94% of the doses administered were noted to be within appropriate dosing ranges per standard of care.19 Additionally, Patrick et al. (2020) noted only one documented medication error amongst 43 prehospital cases, which was found to be related to a change in epinephrine stock concentration due to a drug shortage.20 These cases showcase the safety of push-dose vasopressor administration in the prehospital setting, however prehospital care providers should use great caution when utilizing these agents, as dosing errors can be detrimental.
Paralysis with induction: The use of a neuromuscular blocking agent to induce paralysis is associated with increased likelihood of successful intubation on first attempt. Moiser et al. (2015) showed a nearly 11% increase in first pass success of an endotracheal tube with the use of a paralytic agent in the airway management algorithm.22 NMBAs decrease the risk for regurgitation of the stomach contents which can cause aspiration to be a deadly complication of airway procedures.
The two main classes of paralytic agents include depolarizing and nondepolarizing agents. These agents both induce paralysis of all the skeletal muscles in the body, however, their mechanisms and how they interact with acetylcholine vary.
Depolarizing agents stimulate acetylcholine receptors, which prevent the body’s own acetylcholine from binding with such receptors, allowing the medication to act in place of the body’s own acetylcholine. This stimulation causes muscle depolarization, which then leads to widespread muscle relaxation and muscle paralysis for the duration of action of the depolarizing agent. Depolarizing agents will also cause skeletal muscle fasciculations as the depolarizing agent binds to the acetylcholine receptors, which leads to a release of potassium from cells into the vasculature and can result in an elevated serum potassium level throughout the body.
In contrast, nondepolarizing agents block acetylcholine receptors, and block sodium channels that allow for muscle depolarization. These medications stay bound to the receptors, preventing activation by the body’s own acetylcholine, which induces muscle paralysis. The only depolarizing NMBA that exists is Succinylcholine, nondepolarizing NMBAs commonly used in the prehospital settings include rocuronium and vecuronium.
Providers should consider the pros and cons to each class of medication in this category prior to administration. Succinylcholine is well known for its extensive list of contraindications, including personal history of neuromuscular disease, severe burns, spinal cord damage, CVA, increased intraocular pressure, or end stage renal failure; family or personal history of malignant hyperthermia; or present hyperkalemia. Succinylcholine has been found to raise the serum potassium in a patient as much as 0.5-1.0 mEq after IV administration. This increase in serum potassium can place patients at an increased risk for life threatening arrhythmias, such as high degree heart blocks and Torsades de pointe.
Lastly, longer acting nondepolarizing NMBAs are often neuroprotective in many of the complex neurology and neuro-trauma patients that are transported by prehospital care providers. Movement and the triggering of a gag reflex can cause periodic increases of intracranial pressure, which can be detrimental for these patient populations. The use of an agent such as rocuronium or vecuronium can combat these incidents and lead to safer patient transports.
Induction agents:
Induction agents are medications used to anesthetize patients prior to intubation. Several agents exist, but the most common agents used in the prehospital setting are listed below.
Etomidate: Semi-hypnotic anesthetic medication used as one of the most popular induction agents in both prehospital agencies and healthcare institutions worldwide. Known for its hemodynamic stability and rapid onset, which makes it the preferred induction agent in many areas.
- Dosage: 0.3mg/kg IV push. Max dose 40mg.
- Onset of action: 30 seconds
- Duration of action: 3-5 minutes
- Use with caution in patients with sepsis or adrenal insufficiency due to the adrenal suppression that is associated with Etomidate administration. These patients depend on their adrenal reserves to survive during the acute phase of illness.24 Even one dose of etomidate has been associated with increased mortality in sepsis patients.24
Ketamine: Dissociative anesthetic that works on multiple receptors, most commonly GABA receptors, but also excites opioid receptors that can produce analgesia. Ketamine causes a release of catecholamines, leading to an increase in heart rate, blood pressure, cardiac contractility, and cerebral blood flow.
- Dosage: 2-4mg/kg over two minutes. Studies suggest that dosing should be based off ideal body weight, not actual body weight, to avoid overdose.25
- Onset: 30 seconds-2 minutes
- Duration of action: 20-60 minutes, but may be dose dependent.
- May cause emergence syndrome, which can be characterized by vivid dreams and hallucinations. The use of a low dose benzodiazepine agent in conjunction with ketamine may minimize this emergence reaction.
- Old teachings suggested that ketamine should be avoided in cases of closed head injuries as it can increase intracranial pressure. Despite these teachings, several studies have been conducted that have debunked these mistruths and have addressed the safety and efficacy of ketamine use in the presence of elevated intracranial pressure.
Midazolam: Benzodiazepine that can be used as an induction agent for RSI. Should be used cautiously by prehospital care providers due to the variable effects that it may have on blood pressure.
- Dose: 2.5-5 mg IV or 0.1-0.3mg/kg in pediatrics
- Onset: 30-60 seconds
- Duration of action: 15-30 minutes
- Young neonatal and pediatric patients may require higher doses due to the lower number and undeveloped GABA receptors that Midazolam works on.
Fentanyl: Opioid that is not used as an induction agent but does potentiate induction agents. Prehospital care providers should consider opioid administration to intubated patients, as NMBAs and sedatives do not relieve the pain associated with intubation and positive pressure ventilation. Pain can be characterized by tachycardia and lachrymation in the intubated and paralyzed patient.
- Dosage: 1-3mcg/kg. Repeated every 1-20 minutes as needed.
- Onset: 30 seconds-2 minutes
- Duration of action: 10-20 minutes
- Use caution to ensure that this medication is delivered via slow IV push, especially in young pediatric and neonate patients as they can be prone to rigid chest wall syndrome if pushed rapidly.
Placement with proof: This stage of airway management is one of the most important phases of the entire airway management process, as inadequate verification of placement can lead to detrimental outcomes if endotracheal tube placement is in the wrong position and is not immediately recognized. End tidal carbon dioxide (EtCO2) monitoring is considered the gold standard for endotracheal tube placement, as an adequate quantitative EtCO2 measurement and adequate qualitative EtCO2 waveform is not possible without endotracheal tube placement in the glottic opening.
In addition to placement confirmation, EtCO2 can be used to recognize pulmonary obstructive disease processes, breath stacking, apnea, cardiovascular perfusion status, and wearing off neuromuscular blocking agents, amongst other diagnostic markers. When considering documentation, it is a good idea for the provider to utilize the “snapshot” function of their cardiac monitor to capture the waveform capnography displayed on the monitor. This is an objective measure that documents tube placement confirmation and should be performed after each patient movement.
Post-intubation management: Securement of the endotracheal tube is an important component of post-intubation management. The most commonly employed method of tube securement is a commercial tube securement device that can help to provide stabilization of the endotracheal tube. Providers may also consider the use of a cervical collar to prevent unintentional dislodgement, as they can be used to reduce neck flexion and extension. Tube dislodgement can be one of the most litigious aspects of a transport providers job, so it is essential that transport professionals pay particular attention to tube stabilization.
Continuous sedation and analgesia are additional essential aspects of post-intubation management. Reversing the physiologic process of ventilation by intubation a patient and providing positive pressure ventilation is extremely taxing on the body, thus adequate pharmacological sedation and analgesia should be a priority intervention for these patients. The use of pharmacologic sedatives and analgesics can also help contribute to ventilator synchrony and compliance with positive pressure ventilation.
Basic Airway Management Turned Sideways
Although ventilator management proficiency is not a skill that is maintained by all paramedics across the industry, the use of mechanical ventilation in those that are trained to do so can be beneficial. In using a safe, lung-protective ventilation strategy, patients can be safely ventilated with consistent tidal volumes and targeted metrics. Ventilator settings can be titrated based on vital signs, end tidal capnography values, overall patient condition, and ventilator compliance.
Tracheal damage due to overinflation of endotracheal tube pilot balloons is an avoidable complication of airway management that should be consider. Excessive cuff pressures have been found to cause tissue necrosis and tracheal stenosis when inflated at pressures above 40 cm H20. Monitoring and ensuring endotracheal tube cuff pressures are within a safe range, 20 cm H2O to 30 cm H2O, can help to prevent this adverse complication of intubation.
Patients who have been intubated after periods of extensive noninvasive ventilation, especially pediatric patients, may also benefit from the placement of an orogastric tube. It is common for bag valve mask ventilation and noninvasive ventilation techniques to increase risk for gastric distension. Gastric distension increases the risk for aspiration, and increases intra-abdominal pressure, which can decrease overall cardiac output. Thus evacuation of excess air in the stomach via an orogastric tube can benefit these patients.
Your team successfully prepares for intubation by ensuring the patient is on the full cardiac monitor, has patent IV access, and they assess for possible airway difficulty using the LEMON mnemonic. You ensure that all equipment is assembled, and that all crew members are ready to begin the procedure. The patient is positioned with a pad under the occipital region of the head and their neck extended to optimize laryngoscopy. The patient is adequately preoxygenated and denitrogenated to maximize safe apnea time utilizing a high flow nasal cannula and bag-valve-mask with a PEEP valve and adequate mask seal. While preforming preoxygenation, another paramedic on the team administers a push dose vasopressor to avoid peri-intubation hemodynamic collapse.
Once preoxygenation has completed, and the crew is all ready, the team elects to administer 2mg/kg IBW of ketamine, 1mcg/kg of fentanyl, and 1mg/kg of rocuronium to facilitate the intubation. After the patient is adequately sedated and paralyzed, the intubator uses his video laryngoscope to visualize the endotracheal tube passing through the glottic opening and confirms tube placement using a multifactorial approach that includes qualitative and quantitative end tidal capnography monitoring. The ET tube is secured, and post intubation management follows and includes further sedation and analgesia, continuous ETCO2 monitoring, endotracheal tube cuff pressure monitoring, OG tube placement, and continuous patient monitoring en route to the hospital.
Having a systematic, team-oriented approach to airway management is the key to success when conducting airway management skills in the prehospital setting. As one of the highest acuity but lowest volume skills in the prehospital care provider’s scope of practice, clinicians must keep their skills up to date by practicing the full procedure from start to finish, discuss patient scenarios with other members of their team, and keep themselves apprised of the latest and most up to date research that is ever-evolving.
References
- Hypes CD, Stolz U, Sakles JC, Joshi RR, Natt B, Malo J, Bloom JW, Mosier JM. Video Laryngoscopy Improves Odds of First-Attempt Success at Intubation in the Intensive Care Unit. A Propensity-matched Analysis. Annals of the American Thoracic Society. 2016 Mar;13(3):382-90. doi: 10.1513/AnnalsATS.201508-505OC. PMID: 26653096.
- Wayne MA, McDonnell M. Comparison of traditional versus video laryngoscopy in out-of-hospital tracheal intubation. Prehospital Emergency Care. 2010 Apr-Jun;14(2):278-82. doi: 10.3109/10903120903537189. PMID: 20199237.
- Rezaie Wby S. The heaven criteria part 2 – predicting challenging airways [Internet]. REBEL EM – Emergency Medicine Blog. 2019 [cited 2021Aug27]. Available from: https://rebelem.com/the-heaven-criteria-part-2-predicting-challenging-airways/
- Mort TC. The incidence and risk factors for cardiac arrest during emergency tracheal intubation: A justification for incorporating the ASA guidelines in the remote location [Internet]. Journal of clinical anesthesia. U.S. National Library of Medicine; 2004 [cited 2021Aug27]. Available from: https://pubmed.ncbi.nlm.nih.gov/?term=15590254
- Gnugnoli DM. EMS field intubation [Internet]. StatPearls [Internet]. U.S. National Library of Medicine; 2021 [cited 2021Aug27]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538221/
- Adnet F, Baillard C, Borron SW, Denantes C, Lefebvre L, Galinski M, et al. Randomized study comparing the “sniffing position” with simple head extension for laryngoscopic view in elective surgery patients [Internet]. Anesthesiology. U.S. National Library of Medicine; 2001 [cited 2021Aug27]. Available from: https://pubmed.ncbi.nlm.nih.gov/11605921/
- Schmitz ED. The importance of head positioning during endotracheal intubation [Internet]. EMS Airway. Journal of Emergency Medical Services; 2021 [cited 2021Aug27]. Available from: https://www.emsairway.com/2021/07/27/the-importance-of-head-positioning-during-endotracheal-intubation/#gref
- Colton K. Intubation positioning: Beyond sniffing [Internet]. NUEM Blog. NUEM Blog; 2019 [cited 2021Aug27]. Available from: https://www.nuemblog.com/blog/intubation-positioning
- Khandelwal N, Khorsand S, Mitchell SH, Joffe AM. Head-elevated patient positioning decreases complications of emergent tracheal intubation in the ward and Intensive Care Unit. Anesthesia & Analgesia. 2016;122(4):1101–7.
- Turner JS, Ellender TJ, Okonkwo ER, Stepsis TM, Stevens AC, Sembroski EG, et al. Feasibility of upright patient positioning and intubation success rates at two academic emergency departments. The American Journal of Emergency Medicine. 2017;35(7):986–92.
- Lentz, S., Grossman, A., Koyfman, A., & Long, B. (2020). High-Risk airway management in the Emergency Department. Part I: Diseases and approaches. The Journal of Emergency Medicine, 59(1), 84–95. https://doi.org/10.1016/j.jemermed.2020.05.008
- Long DA, Long B, April MD. Does the use of high-flow nasal cannula compared with conventional oxygen therapy in the peri-intubation period reduce severe desaturation? Annals of Emergency Medicine. 2020;76(3):339–42.
- Nickson C. Preoxygenation [Internet]. Life in the Fast Lane. 2020 [cited 2021Aug27]. Available from: https://litfl.com/preoxygenation/
- Gleason J, Christian B, Barton E. Nasal cannula apneic oxygenation prevents desaturation during endotracheal intubation: An integrative literature review. Western Journal of Emergency Medicine. 2018;19(2):403–11.
- Cole JB, Knack SK, Karl ER, Horton GB, Satpathy R, Driver BE. Human errors and adverse hemodynamic events related to “Push dose pressors” in the emergency department. Journal of Medical Toxicology. 2019;15(4):276–86.
- Nawrocki PS, Poremba M, Lawner BJ. Push Dose Epinephrine use in the management of hypotension during Critical Care Transport. Prehospital Emergency Care. 2019;24(2):188–95.
- Patrick C, Ward B, Anderson J, Fioretti J, Rogers Keene K, Oubre C, et al. Prehospital efficacy and adverse events associated with bolus dose epinephrine in hypotensive patients during ground-based EMS Transport. Prehospital and Disaster Medicine. 2020;35(5):495–500.
- Mosier J, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles J. The physiologically difficult airway. Western Journal of Emergency Medicine. 2015;16(7):1109–17.
- Gagnon DJ, Seder DB. Etomidate in sepsis: understanding the dilemma. Journal of Thoracic Disease. 2015Oct;7(10):1699–701.
- Merelman A, Perlmutter M, Strayer R. Alternatives to rapid sequence intubation: Contemporary airway management with ketamine. Western Journal of Emergency Medicine. 2019;20(3):466-471.
Nicholas Fatolitis, BSN, RN, CEN, CFRN, NRP, FP-C, is a registered nurse and paramedic in the Tampa Bay, FL region. He currently practices as both a flight paramedic for a rotor-based critical care flight team and an emergency department nurse. Nick is also a graduate student at the University of South Florida in an adult-gerontology acute-care nurse practitioner program and works as an adjunct faculty member in the emergency medical services education program at St. Petersburg College.



Good afternoon Nicholas, Very interesting article regarding airway management. We have a mechanical ventilator that is simple to use and very effective. It would give the Paramedic an opportunity to focus on other aspects of patient care during cardiac arrest while maintaining consistent ventilation with the right tidal volume and respirations per min. the device is called the MEDUMAT Easy CPR and I am sure that you would love the concept. As a Paramedic who has worked both prehospital and hospital settings I feel that this device would allow us to provide better patient care during situations where a BVM… Read more »