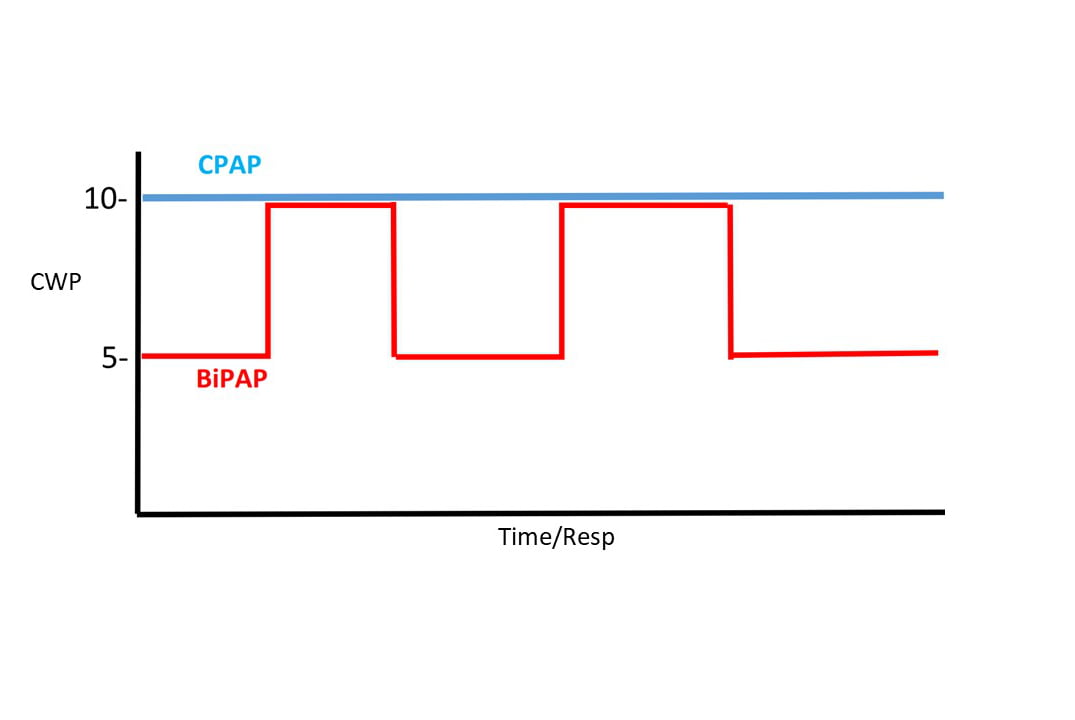
CPAP of 10 CWP compared to BiPAP of 10/5.
Since 2001, continuous positive airway pressure (CPAP) has played an increasingly important role in EMS care for patients who are acutely short of breath, regardless of the cause. CPAP is included in the current EMT, AEMT and paramedic scopes of practice. The introduction of disposable, single-use devices several years ago made CPAP inexpensive and more widely available. As one of the most impactful EMS tools for improving patient outcomes,1 an earlier column, “The Evidence for Prehospital CPAP,” suggested it should be in every EMS toolbox.2 Bilevel positive airway pressure (BiPAP) until recently required a transport ventilator, but is now also available in disposable devices available for EMS. This article reviews the essentials of BiPAP, how it differs from CPAP, and summarizes potential advantages and disadvantages.
Before discussing BiPAP, let’s clear up some semantics. While commonly used to describe bilevel positive airway pressure, the term “BiPAP” is actually a mode delivered by portable ventilators manufactured by Philips Respironics (Murrysville, PA). Another term, “BIPAP” is also a ventilator mode delivered on vents manufactured by Draeger, Inc (Lubeck, Germany). The actual generic term for bilevel positive airway pressure is BPAP. For the sake of familiarity, we’ll use the term BiPAP here, with no specific intent to associate it only with Respironics equipment.
CPAP applies continuous positive pressure to the upper airway, measured in centimeters of water pressure (CWP). This continuous pressure remains the same regardless of whether the patient is inspiring or expiring. While the overall effect of CPAP significantly decreases work of breathing (WOB), there is an increased effort or WOB needed to exhale against CPAP, and the higher the CPAP pressure, the greater the patient effort needed to exhale. The more important effects of CPAP, and the reasons why it is so helpful are splinting open terminal airways thereby improving oxygenation, and lowering transpulmonary pressures resulting in significant reductions in preload and afterload.
The cardiac effects of CPAP make patient improvement seem nearly instantaneous when applied to patients in acute pulmonary edema. The effects in patients with exacerbations of COPD or pneumonia may take considerably longer as it takes time for continuous pressure to recruit collapsed alveoli. Additionally, when higher CPAP pressures are required for effect, the increased work of exhaling against CPAP can become extremely uncomfortable for the patient, and in some individuals, intolerable.
BiPAP, as the bilevel name suggests, delivers two different pressures, inspiratory positive airway pressure (IPAP) and a lower, expiratory positive airway pressure (EPAP). This allows a higher pressure to be delivered during inspiration, and a lower pressure during expiration, thereby reducing the work of exhaling. The difference between the pressures, a value called pressure support (PS) or Delta P, is directly related to tidal volume. (See Why Not BiPAP?). The greater the difference in pressures, the higher the patient’s tidal volume will be. The ability of BiPAP to increase tidal volumes and therefore, lower CO2 levels, is what most differentiates it from CPAP.
The weight of evidence supporting use of CPAP for virtually any type of acute respiratory distress encountered in the prehospital environment strongly suggests it is likely to benefit the majority of patients. BiPAP offers the same support as CPAP with the added ability to further decrease work of breathing during exhalation and improve tidal volumes thereby clearing more CO2 than CPAP. It is a reasonable alternative for patients who are unable to tolerate CPAP, those who require high CPAP pressures, and for patient’s whose respiratory failure is primarily related to hypercarbia (high CO2 levels).
There are some disadvantages associated with BiPAP, the most significant of which is apnea induced by higher levels of pressure support than a patient requires. This can occur on initial setup, or as a patient’s respiratory status recovers during EMS care. Ventilators and machines configured to deliver BiPAP all monitor respiratory rates and, if they detect apnea, begin mechanical ventilation4-6. Such monitoring and backup support is not available on disposable BiPAP units; EMS providers must remain hyper vigilant whenever using BiPAP without respiratory rate monitoring and apnea ventilation capability.
An additional disadvantage of BiPAP is the knowledge and skill needed to select and subsequently adjust the IPAP and EPAP settings. IPAP is always set higher than the EPAP; most references suggest an initial IPAP setting of 8 – 10 CWP and EPAP of 3- 5 CWP. Increasing the IPAP will clear more CO2 whereas increasing the EPAP will improve oxygenation (in the same fashion as increasing CPAP pressures improve oxygenation). Patients who are intolerant of high EPAP levels may benefit from increasing their IPAP.
The non-invasive ventilation tool most commonly used in hospitals has increasingly become available to prehospital providers. Familiarity with BiPAP equipment, the differences between CPAP and BiPAP, and the situations where BiPAP might be useful are important. Equally imperative is an understanding of how to set and titrate IPAP and EPAP as well as an appreciation for the advantages and disadvantages BiPAP offers. In most situations, CPAP is a familiar and comfortable starting point when managing a patient with acute respiratory distress. BiPAP might fill a void for some of those patients and, in the right circumstances with the right equipment, has potential to offer better outcomes.
References
- Myers JB, Slovis CM, Eckstein M, Goodloe JM, Isaacs SM, Loflin JR, Mechem CC, Richmond NJ, and Pepe PE. Evidence-Based Performance Measures for Emergency Medical Services Systems: A Model for Expanded EMS Benchmarking. Prehospital Emergency Care. 2008;12:141-151.
- Roessler MS, Schmid DS, Michels P, et al. Early out-of-hospital non-invasive ventilation is superior to standard medical treatment in patients with acute respiratory failure: a pilot study. Emerg Med J 2012; 29:409.
- Ferguson GT, Gilmartin M. CO2 rebreathing during BiPAP ventilatory assistance. Am J Respir Crit Care Med 1995; 151:1126.
- Liesching T, Kwok H, Hill NS. Acute applications of noninvasive positive pressure ventilation. Chest 2003; 124:699.
- Kacmarek, RM. Characteristics of pressure-targeted ventilators used for noninvasive positive pressure ventilation. Respir Care 1997; 42:380.
- Ferguson GT, Gilmartin M. CO2 rebreathing during BiPAP ventilatory assistance. Am J Respir Crit Care Med 1995; 151:1126.
Mike McEvoy, PhD, NRP, RN, CCRN, is the EMS coordinator for Saratoga County, New York, and the professional development coordinator for Clifton Park and Halfmoon Ambulance. He is a nurse clinician in the adult and pediatric cardiac surgery intensive care units at Albany Medical Center, where he also teaches critical care medicine. McEvoy is the chief medical officer and firefighter/paramedic for West Crescent Fire Department in Clifton, New York. He is also the chair of the EMS Section board of directors for the International Association of Fire Chiefs and a member of the New York State Governor’s EMS Advisory Council. He is a lead author of the textbook Critical Care Transport, the “Informed” Pocket References (Jones & Bartlett), and the American Academy of Pediatrics textbook Pediatric Education for Prehospital Professionals (PEPP).


