By Mike McEvoy, PhD, NRP, RN, CCRN
Shortness of breath, or dyspnea, results from air hunger, a sensation that you’re not getting enough air. Healthcare providers often incorrectly associate dyspnea with hypoxia (i.e., lack of oxygen). In fact, healthy patients who become hypoxic don’t experience shortness of breath.
Most commercial airline cabins can’t be pressurized to normal sea level atmospheric pressures, resulting in average oxygen saturations of 88.6% in airline passengers, typically with no ill effects. In planes that suddenly depressurize, passengers typically lose consciousness at oxygen saturations below 56%. Few experience any shortness of breath or other symptoms prior to passing out, which is why airline pilots are discouraged from flying unpressurized aircraft at high altitudes without supplemental oxygen.1–3
Air Hungry
Our drive to breathe actually results from carbon dioxide (CO2). When there are increased levels of CO2 in the lungs or bloodstream, we experience air hunger. Normally, our bodies adjust respiratory rate and depth to maintain an arterial level of CO2 close to 40 mmHg. CO2 then, whether measured in the blood or in exhaled breaths, is a useful marker for respiratory status and helpful for determining the severity of dyspnea. A person who is air hungry will work harder to breathe, and expend more energy doing so. In addition to CO2, work of breathing (WOB) is an important assessment for an EMS provider evaluating a patient with dyspnea.
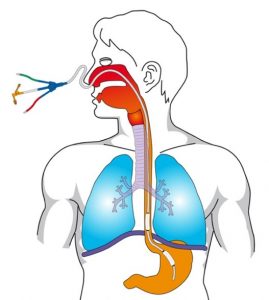
A gastroesophageal balloon catheter used to measure transpulmonary pressures.
Traditionally, respiratory rate has been used as a surrogate for work of breathing. Depending on what textbook you reference, significantly increased WOB was thought to be present in adults at respiratory rates above 30 or 40 per minute. Over time, research in critical care patients has downplayed the reliability of respiratory rate.
Currently, transpulmonary pressure is considered to be the most reliable WOB assessment tool. Measured in joules per liter or in joules per minute, WOB can be calculated by multiplying pressure and volume measurements obtained from a gastroesophageal balloon catheter. Although helpful for predicting successful ventilator weaning in a critical care setting, it’s highly impractical for use outside of an ICU.
What to Look For
Considering the four factors that commonly increase WOB, it’s possible to target our assessment of patients increased WOB in the field. These four factors result in predictable physical exam findings, if you know to look for them:
- A need for increased ventilation (i.e., exchange of gases);
- Increased airway resistance;
- Decreased pulmonary (i.e., lung) compliance; and
- Decreased lung elastic recoil.
Increased WOB often results in visible retractions of muscles in the neck and chest, nasal flaring (particularly in children and infants), pursed-lip breathing and changes in posture such as sitting upright and leaning forward using the arms to support the chest wall muscles. If the respiratory muscle load exceeds breathing capacity, exhaled levels of CO2 will increase.
In a patient without chronic obstructive lung disease (COPD), the textbook definition of respiratory failure is a CO2 level above 70 mmHg (blood or exhaled). This suggests a need for ventilator assistance. A similar effect occurs with oxygenation and is readily apparent in patients not receiving supplemental oxygen. Once WOB exceeds the capacity of the patient to move air, SpO2 will begin to fall. Often, the administration of supplemental oxygen conceals this important finding. This is one good reason not to administer supplemental oxygen to patients with normal oxygen saturations.
Level of consciousness also correlates well with WOB. Patients who are acutely short of breath with significantly increased WOB may become extremely anxious or, especially when CO2 rises, become obtunded or sleepy. A dyspneic patient who becomes acutely agitated may be well on the way to respiratory arrest.
Subjective assessments are very important and should always be considered. Asking a patient to rate their difficulty breathing or their perception of how much they are exerting themselves to breathe on a scale from zero to 10 can be very helpful initially, during and after treatment. These rating systems are often referred to as Borg scales.
Using Clinical Judgement
Finally, clinical judgement can’t be overemphasized. Medicine, especially pulmonary medicine, is as much an art as it is a science. There are no hard and fast rules for treating patients with acute shortness of breath.
The psychological components of not being able to breathe can significantly exacerbate and often confuse assessment of the physical causes of dyspnea. Past experience, knowledge of the individual patient, and careful ongoing assessment using all the tools available help providers to address the causes of acute shortness of breath and hopefully, to not only prevent deterioration, but improve the clinical picture for the patient.
References
- Akero A, Christensen CC, Edvardsen A, et al. Hypoxaemia in chronic obstructive pulmonary disease patients during a commercial flight. Eur Respir J. 2005;25:725-730.
- Cottrell JJ, Lebovitz BL, Fennell RG, et al. In flight arterial saturation: Continuous monitoring by pulse oximetry. Aviation Space and Environmental Medicine. 1995;66:40–44.
- Hoffman CE, Clark RT Jr, Brown EB Jr. Blood oxygen saturations and duration of consciousness in anoxia at high altitudes. Am J Physiol. 1946;145:685–692.
- Bellani G, Pesenti A. Assessing effort and work of breathing. Current Opinion in Critical Care. 2014;20:352-358.
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381.
Mike McEvoy, PhD, NRP, RN, CCRN, is the EMS coordinator for Saratoga County, New York, and the professional development coordinator for Clifton Park and Halfmoon Ambulance. He is a nurse clinician in the adult and pediatric cardiac surgery intensive care units at Albany Medical Center, where he also teaches critical care medicine. McEvoy is the chief medical officer and firefighter/paramedic for West Crescent Fire Department in Clifton, New York. He is also the chair of the EMS Section board of directors for the International Association of Fire Chiefs and a member of the New York State Governor’s EMS Advisory Council. He is a lead author of the textbook Critical Care Transport, the “Informed” Pocket References (Jones & Bartlett), and the American Academy of Pediatrics textbook Pediatric Education for Prehospital Professionals (PEPP).


