The Miracle of CPAP
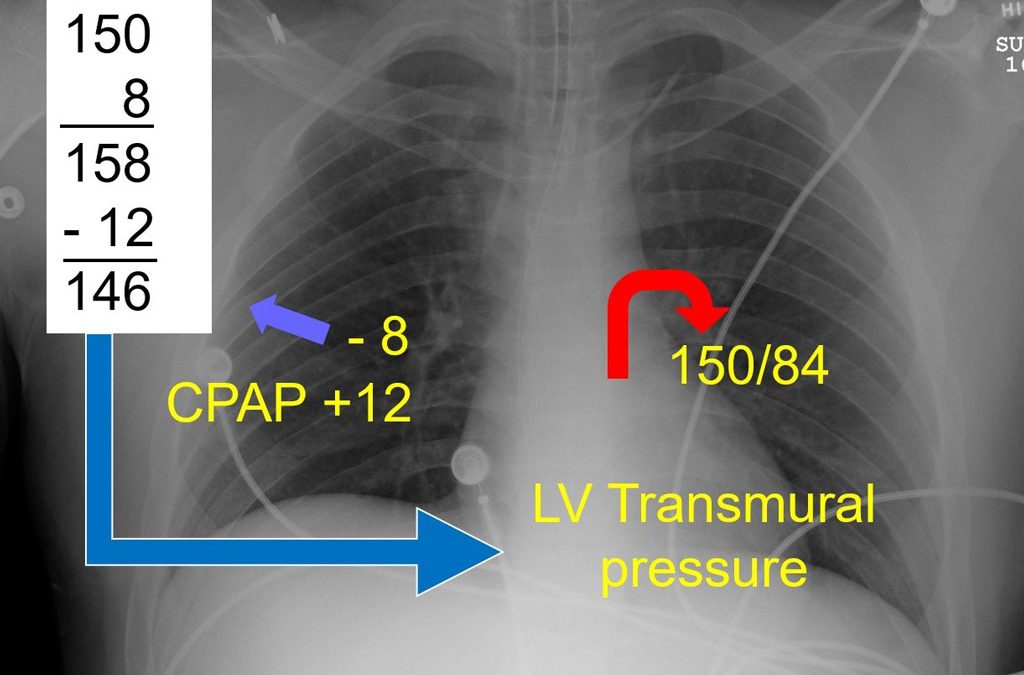
Mike McEvoy examines some of the physiological reasons that continuous positive airway pressure (CPAP) works for a variety of conditions.
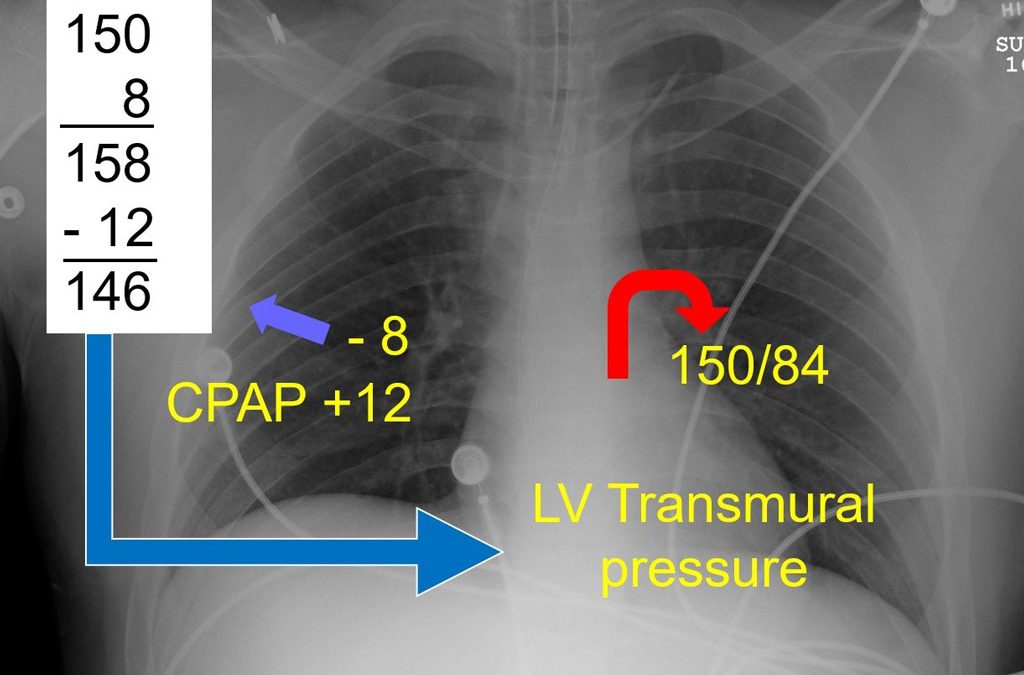
Mike McEvoy examines some of the physiological reasons that continuous positive airway pressure (CPAP) works for a variety of conditions.

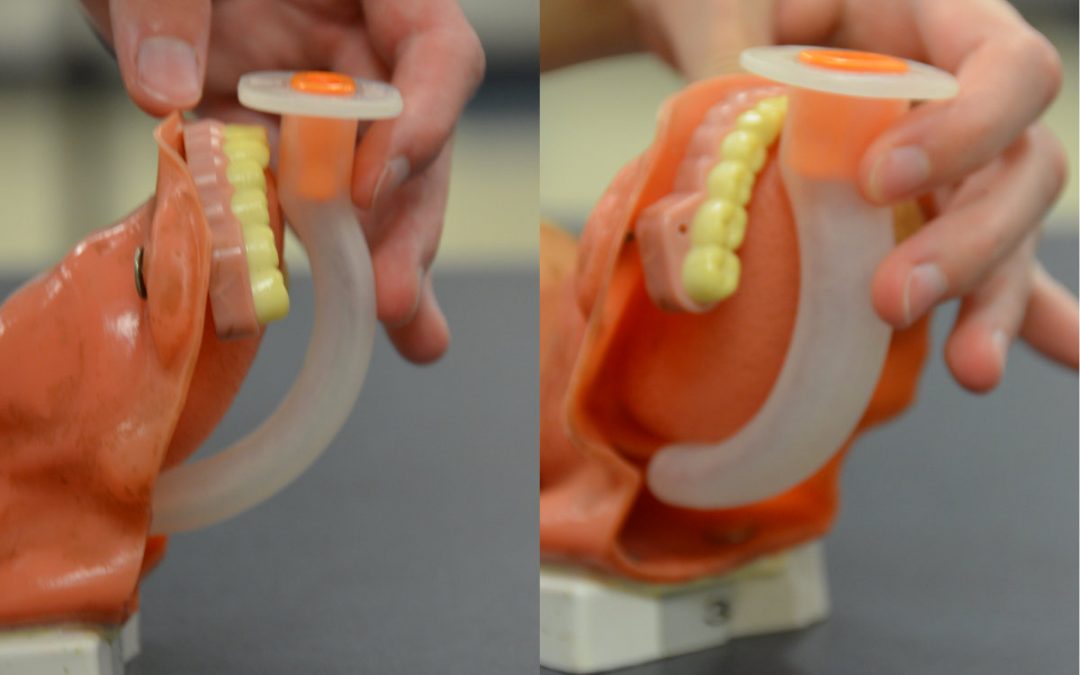
In this video, Mike McEvoy discusses the use of disposable CPAP (continuous positive airway pressure) masks, a method of assisting a patient’s respiration without intubation.

Barriers to CPAP adoption by BLS providers are finally falling, and BLS use of CPAP is now supported by the 2019 National EMS Scope of Practice Model.

Although originally intended to treat prehospital patients in pulmonary edema resulting from heart failure, CPAP is now indicated for virtually any condition resulting in significant dyspnea accompanied by signs and symptoms of increased work of breathing.
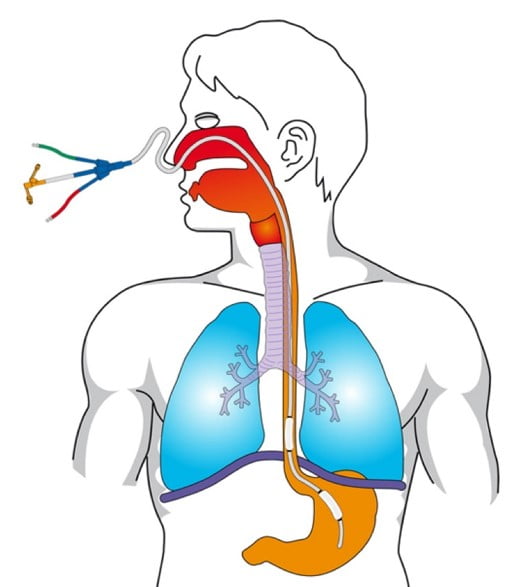
Learn the history of the oropharyngeal airway (OPA) and review how to size the OPA for the patient, as well as the correct way to insert this basic, and effective, airway adjunct.
Shortness of breath, or dyspnea, results from air hunger, a sensation that you’re not getting enough air. Here’s how to spot a patient with increased work of breathing, an important assessment for an EMS provider evaluating a patient with dyspnea.
Recent Comments