By Jairo Chavez Jr.
Abstract
In the evolving landscape of prehospital care, precision in airway management is no longer optional—it’s essential. This article outlines how optimizing tidal volume using patient height and ideal body weight (IBW), alongside the capabilities of the ZOLL BVM (bag-valve-mask) Assist, can significantly improve outcomes in cardiac arrest resuscitation.
Purpose
The purpose of this article is to improve the way we approach ventilating patients. In the last year and a half, we have progressed in our competency with the ZOLL (BVM) assist. EMTs and paramedics across Omaha, Nebraska, have become proficient at delivering adequate ventilation in volume and rate.
We would like to take the opportunity to push everyone one step forward in improving ventilations by focusing on ideal tidal volume based on the patient’s height and ideal body weight. These steps will coordinate with our advanced cardiac resuscitation (ACR) goals of improving patient outcomes in cardiac arrest.
Anatomy and Physiology Review
Common EMS sayings like “more air is better” or “bigger patient, bigger breath” have persisted for years, but they often lead to overventilation and unintended harm. Yet, as we advance our understanding of cardiopulmonary physiology, it’s clear that this mindset can be counterproductive—especially during cardiac arrest.
In the past 18 months, Omaha (NE) Fire Department personnel have made considerable strides in using the ZOLL BVM Assist to standardize ventilation rates and volumes. Now, it’s time to push further by integrating ideal tidal volume (ITV) into our practice.
Two phrases we may have heard before in our career that have become a misnomer. Every day we see patients of all shapes and sizes. When it comes to ventilating these patients, we may default to those phrases or rely on visual confirmation of chest rise.
Hyperventilation—both in rate and volume—remains a significant issue in prehospital care. Excessive tidal volumes increase intrathoracic pressure, reduce venous return, and decrease cardiac output. These effects run counter to the goals of advanced cardiac resuscitation (ACR), particularly Phase II, which emphasizes minimizing intrathoracic pressure and enhancing cerebral perfusion.
In one hospital study, over 72% of nurses, physicians, and patients (self-reported) overestimated patient heights. These heights are used to calculate a patient’s IBW and then determine an ideal tidal volume (ITV) of 6–8 mL/kg.1
Using patient height to calculate IBW allows EMS clinicians to determine a more physiologically appropriate ITV:
- 6–8 mL/kg of IBW.
- Avoids overinflation and supports better cardiac perfusion during CPR.
Height and ideal body weight are used as a more reliable way to measure the appropriate tidal volume. Greater body weight doesn’t mean larger lungs. (Lung size correlates more with height than with weight.) Another way to think about it: A 6-foot male weighing 180 pounds and a 6-foot male weighing 300 pounds should receive the same tidal volume. They have similar lung volumes, not based on weight, but height.
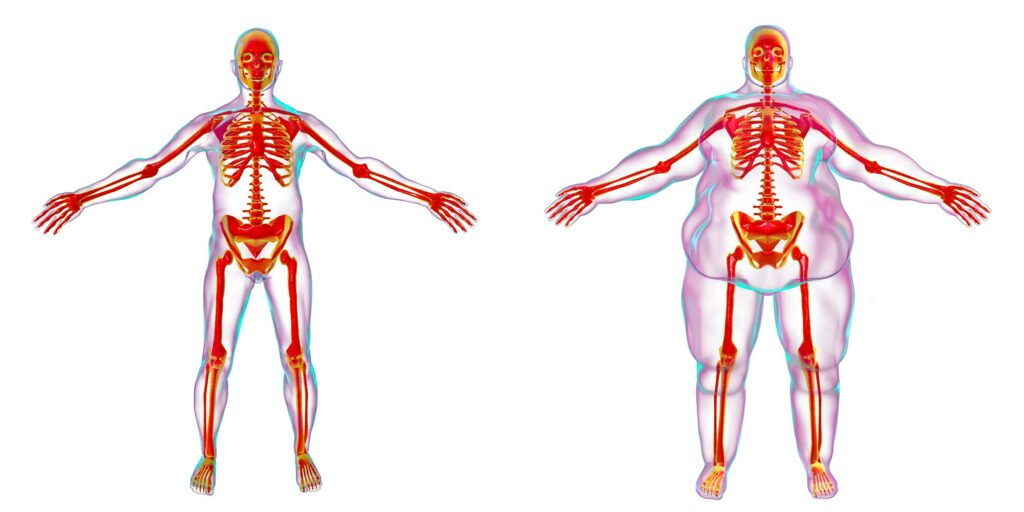
DepositPhotos/Kateryna-Kon
ACR goal: When it comes to improving patient outcomes, there has been emphasis on four different pressures:
- Increasing coronary perfusion pressure.
- Decreasing intrathoracic pressure.
- Increasing cerebral perfusion pressure.
- Decreasing intracranial pressure.
In Phase I, the focus was on continuous uninterrupted compressions. This stage improved our chest compression fraction (CCF), which improved our coronary perfusion pressure and cerebral perfusion pressure. In Phase II, smaller details will be implemented to decrease intrathoracic pressure (tidal volume) and decrease intracranial pressure (head elevation).
Ventilations and tidal volume are metrics we can now measure and control via the ZOLL BVM Assist. Larger tidal volumes during cardiac arrest hinders our goals of ACR. Large tidal volumes, compared to ideal tidal volume (Fig. 1), create an increase in intrathoracic pressure as a result, decreasing cardiac output (Fig. 2).
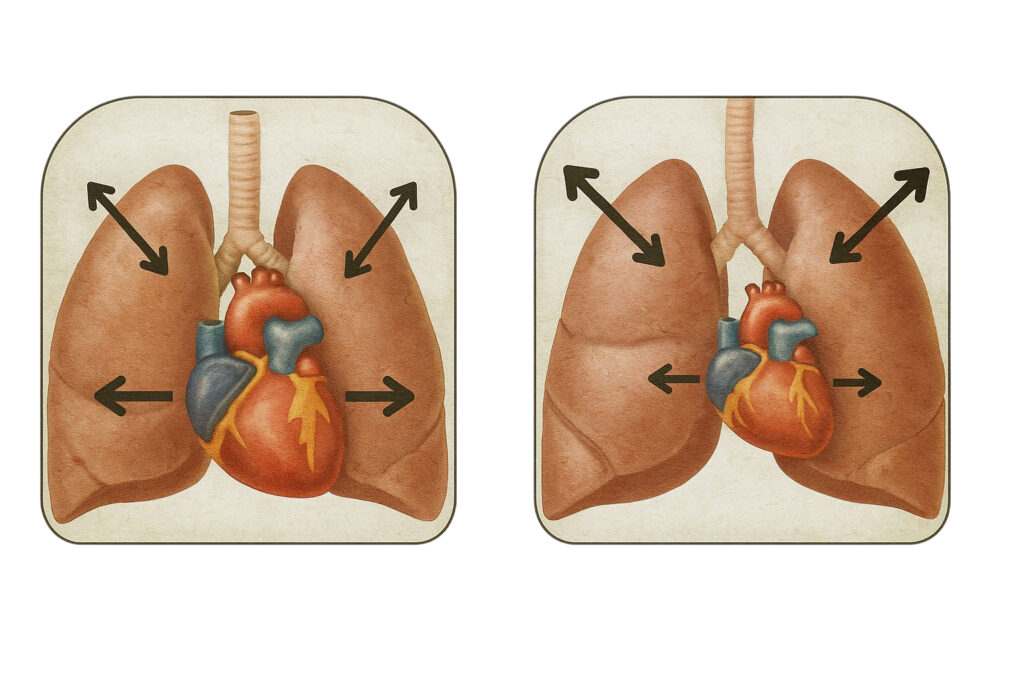
Figure 1: Ideal Tidal Volume: Less intrathoracic pressure is produced allowing the heart to fully contract and refill, increasing cardiac output. Figure 2: Large Tidal Volume: More intrathoracic pressure is produced resulting in more pressure on the heart and decreasing cardiac output. (AI images created by the author.)
Calculations
The estimated ideal body weight of a patient, calculated using the following calculations based on their height:
IBWMale = 50 kg + 2.3(Height in inches – 60)
IBWFemale = 45.5 kg + 2.3(Height in inches – 60)
ITV is then calculated based on 6–8 mL/kg (IBW)2
These small adjustments can yield big outcomes in Phase II of ACR, where subtle physiologic wins, like lowering intracranial and intrathoracic pressures, translate into increased survivability.
Real-World Application Made Simple
While calculating IBW during a high-stakes code may seem impractical, field-friendly tools make it easier:
- Use the Cot: Most stretchers measure 74–81 inches long. Visually estimate how the patient fits to approximate height.
- Use IDs: Many patient IDs list height.
- Preset Guidance: The ZOLL BVM Assist default is 450 mL. For an average male (5’9”), this equals ~6.4 mL/kg—ideal. But for the average female (5’4”), that same 450 mL equals ~8.2 mL/kg—too high.
➡ Adjustment Tip: Use the tidal volume/height chart provided to determine more appropriate settings.
It may seem daunting to try and calculate all that during a code. That is why the chart below has been created to help calculate and set your tidal volume to an appropriate dose.
Helpful Hint: Studies have proven we are not the greatest at estimating a patient’s weight.
The same goes for estimating a patient’s height. One trick you can use is your cot. If your patient is placed supine on the cot, how much space is left (from top and/or bottom) or how much is the patient hanging over? The cot mattress measures 74 inches. The overall length of the entire cot is 81 inches. You may get a closer estimate when using a reference to measure. If possible, you can also use the height listed on someone’s ID.
Example: The average adult male in the United States is 5’9”. Using the chart below, that would give us an ideal tidal volume (6–8 mL/kg IDW) of 424–547 mL per ventilation. The average adult female is 5’4”. The ideal tidal volume would be 328–438 mL per ventilation.
To put that in perspective, the ZOLL X Series is set to a default of 450 mL when using the BVM assist. For the average adult male, at 450 mL, we are giving approximately 6.4 mL/kg. For the average adult female, at 450 mL, we are giving approximately 8.2 mL/kg.
The volume is within an acceptable range for the average adult male, but too high for the average adult female. Therefore, adjustments should be made to be within an acceptable range while considering the effects the tidal volume will have on the overall intrathoracic pressure and cardiac perfusion pressure.
Small Goal: This isn’t meant to be perfect, but it is meant to help us get closer to a target and improve our approach. Hairs can be split over whether a female patient is 5’3 or 5’4 but overall if an adjustment is made to give a tidal volume of 314–328 mL, we will be better off than if we gave a tidal volume of 450.
| Predicted Ideal Body Weight / Tidal Volume | ||||||||||
| Males | Females | |||||||||
| Height | IBW | 6 mL/Kg | 8 mL/Kg | Height | IBW | 6 mL/Kg | 8 mL/Kg | |||
| Feet | Inches | Feet | Inches | |||||||
| 5’0 | 60 | 50 | 300 | 400 | 4’8 | 56 | 36.3 | 218 | 290 | |
| 5’1 | 61 | 52.3 | 314 | 418 | 4’9 | 57 | 38.6 | 232 | 309 | |
| 5’2 | 62 | 54.6 | 328 | 437 | 4’10 | 58 | 40.9 | 245 | 327 | |
| 5’3 | 63 | 56.9 | 341 | 455 | 4’11 | 59 | 43.2 | 259 | 346 | |
| 5’4 | 64 | 59.2 | 355 | 474 | 5’0 | 60 | 45.5 | 273 | 364 | |
| 5’5 | 65 | 61.5 | 369 | 492 | 5’1 | 61 | 47.8 | 287 | 382 | |
| 5’6 | 66 | 63.8 | 383 | 510 | 5’2 | 62 | 50.1 | 301 | 401 | |
| 5’7 | 67 | 66.1 | 397 | 529 | 5’3 | 63 | 52.4 | 314 | 419 | |
| 5’8 | 68 | 68.4 | 410 | 547 | 5’4 | 64 | 54.7 | 328 | 438 | |
| 5’9 | 69 | 70.7 | 424 | 566 | 5’5 | 65 | 57 | 342 | 456 | |
| 5’10 | 70 | 73 | 438 | 584 | 5’6 | 66 | 59.3 | 356 | 474 | |
| 5’11 | 71 | 75.3 | 452 | 602 | 5’7 | 67 | 61.6 | 370 | 493 | |
| 6’0 | 72 | 77.6 | 466 | 621 | 5’8 | 68 | 63.9 | 383 | 511 | |
| 6’1 | 73 | 79.9 | 479 | 639 | 5’9 | 69 | 66.2 | 397 | 530 | |
| 6’2 | 74 | 82.2 | 493 | 658 | 5’10 | 70 | 68.5 | 411 | 548 | |
| 6’3 | 75 | 84.5 | 507 | 676 | 5’11 | 71 | 70.8 | 425 | 566 | |
| 6’4 | 76 | 86.8 | 521 | 694 | 6’0 | 72 | 73.1 | 439 | 585 | |
| 6’5 | 77 | 89.1 | 535 | 713 | 6’1 | 73 | 75.4 | 452 | 603 | |
| 6’6 | 78 | 91.4 | 548 | 731 | 6’2 | 74 | 77.7 | 466 | 622 | |
| 6’7 | 79 | 93.7 | 562 | 750 | 6’3 | 75 | 80 | 480 | 640 | |
| 6’8 | 80 | 96 | 576 | 768 | 6’4 | 76 | 82.3 | 494 | 658 | |
| 6’9 | 81 | 98.3 | 590 | 786 | 6’5 | 77 | 84.6 | 508 | 677 | |
| 6’10 | 82 | 100.6 | 604 | 805 | 6’6 | 78 | 86.9 | 521 | 695 | |
| 6’11 | 83 | 102.9 | 617 | 823 | 6’7 | 79 | 89.2 | 535 | 714 | |
| 7’0 | 84 | 105.2 | 631 | 842 | 6’8 | 80 | 91.5 | 549 | 732 | |
Table 1: Tidal Volume Chart.
Real-Time Adjustments
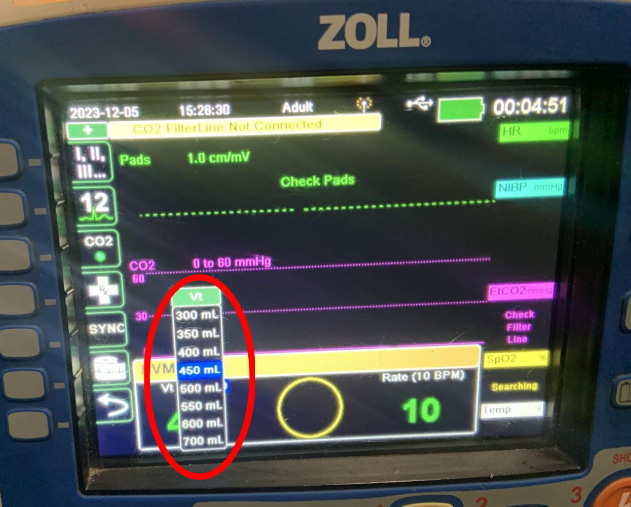
Depending on your volume goal, a tidal volume adjustment may not be necessary each time. ZOLL X Series allows adjustments made in increments of 50 mL. The program is also designed to give you a volume reading with each ventilation. It also gives you a green number when within ± 50 mL of the preset volume (450 mL).
When you make an adjustment to the preset, consider using a preset closer to your determined ideal tidal volume.
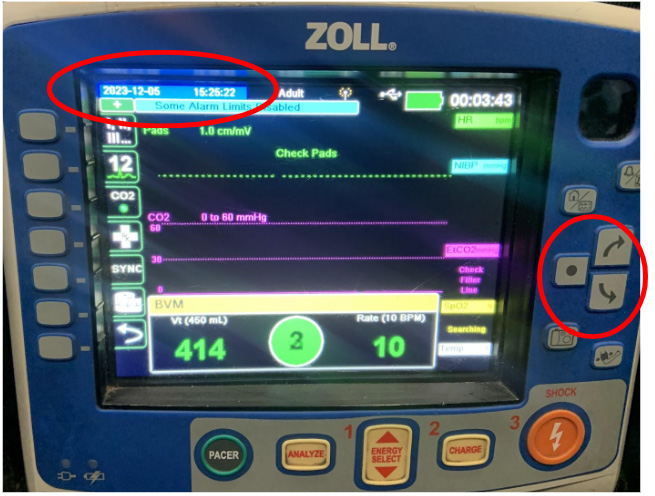
Author photo.
To change the desired preset, find the highlighted item on the monitor (see photo). Use the arrows on the right side of the monitor to move the highlighted portion to the “Vt” under the BVM. Once highlighted (see below), use the “⚫” to select.
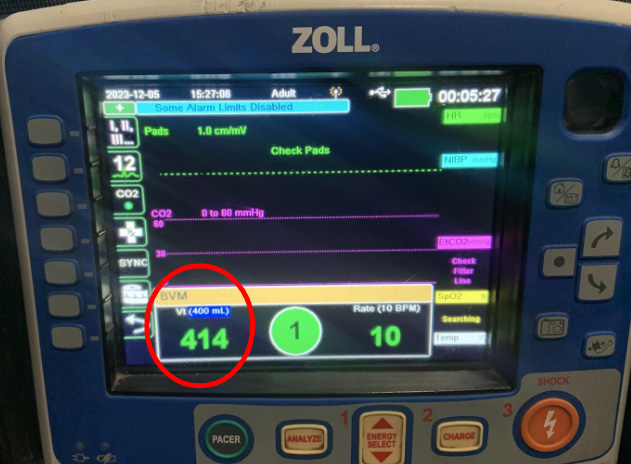
Author photo.
Author photo.
Once selected, the preset tidal volume can be changed as desired. The same steps can be performed to adjust the desired ventilation rate, by highlighting and selecting “Rate.”
Capnography Consideration
Real-time end-tidal CO₂ values are critical indicators of perfusion, and ventilation quality has played a major role in determining the effectiveness of cardiac resuscitation. A normal, healthy range is 35–45 mmHg.
Omaha (NE) Fire Department’s (OFD) recent code data have shown end-tidals in the 50- to 60-foot range, and some well above that. The American Heart Association considers anything between 10 and 20 as adequate during resuscitation. With the ACR Phase I, OFD is exceeding the adequate standards of AHA.
Real-time adjustments can continue as resuscitation progresses. This begins with adjustments to tidal volume to decrease intrathoracic pressure and improve cardiac output. Once resuscitation efforts hit that lull or comfortable state of “what to do next?” Hs and Ts considerations should be next.
When considering acidosis and EtCO2, maybe now it’s time to make adjustments to the ventilation rate to aim for a normal range. If EtCO2 is high, you may increase and tailor the rate slowly to decrease EtCO2. If EtCO2 is low, you may consider decreasing the rate to increase EtCO2.
If ↑ EtCO2 (too high) = ↑ Ventilation Rate to decrease EtCO2
If ↓ EtCO2 (too low) = ↓ Ventilation Rate to increase EtCO2
Operational Takeaways
- Tidal volume adjustments should be tailored, not guessed.
- Use the monitor. Treat the patient and the monitor.
- Balance science with intuition. Medicine is an art informed by real-time data.
Conclusion
As prehospital clinicians, we’ve refined our skills in compressions, defibrillation, and drug administration—but ventilation still deserves precision.
By combining height-based tidal volume calculations with the real-time feedback of the ZOLL BVM Assist, we can align ventilation practices with our ACR goals. Treat the patient, yes—but when the monitor speaks, let it guide you. Precision saves lives.
About the Author
Jairo Chavez is a fire apparatus engineer and paramedic with the Omaha (NE) Fire Department, where he has proudly served since 2017. He is currently assigned to Truck 41 and brings a strong instructional background through his role as an EMS educator with Creighton University since 2017. Chavez has a bachelor’s degree in emergency medical services from Creighton University and an associate’s degree in fire science from Metropolitan Community College. His professional interests include advancing prehospital care, improving patient outcomes, and exploring innovations in field-based resuscitation practices.
References
1. Alexandre AR, Rocha FR, Landeiro L, Mota P, Jones J, Gomes JA. Impact of height estimation on tidal volume calculation for protective ventilation—a prospective observational study. Critical Care Explorations. 2021 May;3(5). doi:10.1097/cce.0000000000000422.
2. O’Brien ID, Shacklock E, Middleditch A, Bigham C. Inaccuracies in calculating predicted body weight and its impact on safe ventilator settings. J Intensive Care Soc. 2016 Aug;17(3):191-195. doi: 10.1177/1751143715626163. Epub 2016 Feb 9. PMID: 28979490; PMCID: PMC5606514.
Exclusive feature content from thought leaders in airway management.


