Photo illustrations created by the author.
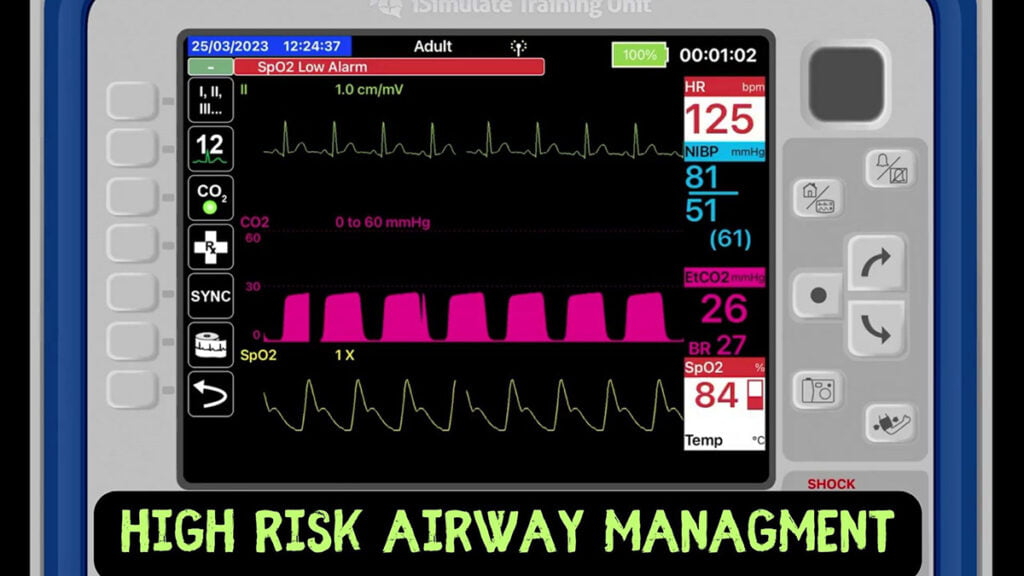
What is high-risk airway management (HRAM)? It is exactly the stuff nightmares are made of: Patients who present to us, outside of the hospital, with severe injuries and competing treatment priorities.
Performing RSI on these patients is a lot like walking alone down a scary alleyway in the big city.
It looks something like this:

In Part 1, we established that HRAM does not begin and end with a view of the vocal cords and the passage of the endotracheal tube. In fact, in trauma cases and other high-risk situations, the passage of the tube may be one of the least important tasks that is accomplished, especially if it is done with inattention to the patient’s hemodynamic instability.
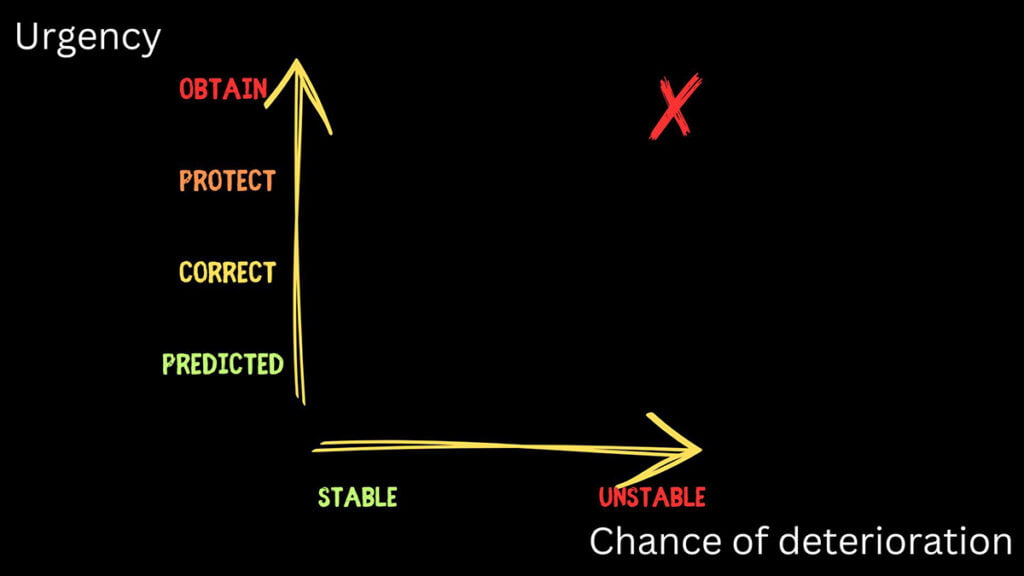
In fact, hypotension may be the biggest risk factor of all. These are patients that are at the top of the scale for complications and danger. They need an airway, but not just an airway. They need some resuscitation and then an intubation.
The Problem: Hypotension Contributing to Cardiac Arrest
Hypotension is the monster in your closet in this situation. It is an independent predictor of cardiac arrest following intubation, which is where we will focus most of our attention. If we ignore it or fail to adequately respond to it, there is a high risk of cardiac arrest. While the prehospital data on this is sparse, there is plenty of literature we can extrapolate from the in-hospital environment.
Hypotension
Hypotension is present in many of our trauma patients who require intubation. Let’s not forget that hypotension is a late sign of shock and indicating that your patient is decompensating. They are running out of physiologic time and reserve to continue to sustain normal homeostatic function.
They are incredibly hemodynamically fragile. Is the hypotension only coming from the ongoing hemorrhage? What if it is iatrogenic, meaning we are causing it (with our best of intentions)?
Preload Problems:
- Volume depletion from ongoing hemorrhage
- PPV from BVM to pre-oxygenate the patient
- Induction agent administration
- Venous pooling from paralytics
Afterload Problems:
- Use of bolus dose vasopressors in low volume states. Leading to vasoconstriction, but not necessarily better cardiac output.
Contractility Problems:
- Low volume due to hemorrhage (no stretch)
- Induction agents that cause myocardial suppression
So, it could be any number of things. What does the evidence say? Is this really all that common of an issue?
Heffner et al. looked in to the frequency and significance of hypotension in emergency airway management. A total of 336 cases were studied and found 23% (79 patients) experienced post intubation hypotension and these patients had worse in-hospital mortality (33% did not survive) or a longer stay in the hospital (also associated with more morbidity and mortality). A total of 96% (76 patients) were hypotensive before intubation.
Heffner et al. also looked in to the predictors of postintubation hypotension and cardiovascular collapse in airway management. In that study, 300 cases were evaluated and in 66 of them, a higher incidence of mortality was noted. The primary culprit was a pre-intubation shock index of 0.8 or higher, in fact this data point comes with 80% specificity. That is high enough that if you see it on scene, you need to take deliberate actions to address it.
Peri/Post-Intubation Cardiac Arrest (PICA)
Why all of this focus on hypotension? Aren’t we intubating the patient for airway protection or to correct hypoxia? Of course, those are indications for intubation, but as we have been unpacking the data, we should be seeing that how we execute this procedure can add to the danger and instability
Wardi et al. evaluated the association of hypotension and airway management in the ICU over a five-year period. A total 29 of the patients in this study experienced PICA (post-intubation cardiac arrest), and of those patients, 52% (or 15 patients) died. An independent predictor of PICA that we can extrapolate to the prehospital environment was a shock index >1.0. Other predictors were intubation within an hour of shift change and the use of succinylcholine as the paralytic.
De Jong et al. performed another ICU level evaluation of PICA that found an incidence of 2.7% (49 patients out of 1,847) that showed a 28.6% mortality rate (71% achieved ROSC). The main predictor? Hypotension (SBP < 90). Interestingly they could not replicate succinylcholine use as an independent predictor of PICA.
The NEAR study looked at intubation in multiple emergency departments, specifically the incidence of PICA. 157 patients, roughly 1% of the study population experienced PICA. Of those 157 patients, 32% (50 or so patients) did not survive. Again, the largest predictor of PICA was hypotension (defined in this study as SBP < 100).
Looking at these numbers, the evidence would lead us to believe that PICA is relatively rare. The chances of something happening 1-5% of the time is a risk we are willing to take, right? The problem is that the mortality in these groups is exceedingly high, as low as 30% and as high as 52%.
Meaning, that the risk of the patient going in to cardiac arrest during intubation is pretty low, but the chances of them not surviving that arrest is high enough for us to make every attempt to avoid a PICA event, at all costs.
Conclusions
Intubating a hypotensive trauma patient is wrought with hurdles and pitfalls. So much so, that if we trip over one of them, there is a good chance of a poor outcome for the patient. Some systems have a large toolbox for how to address the physiologic difficulties of managing trauma patient’s airways, and others do not.
In Part 3 we will unpack some clinical bundles that have been implemented across the country to address many of the issues identified in this article.
Cody Winniford is a flight paramedic and base manager in Baltimore, MD. He has a passion for sharing his professional experience in EMS and management. Cody’s clinical and leadership development background spans both military and civilian settings and has served in several capacities as a leader and prehospital clinician. He specializes in air medical and critical care transport, as well as organizational development and leadership development. He is an active speaker on various leadership and clinical topics and is an established and successful educator for prehospital clinicians of all levels. He has a passion for human performance improvement and the mental health and performance aspects of prehospital care.


