
Photo compliments to photographer Robert Bryant, NRP, and Matthew Hajek, EMT, Dorchester County (SC) EMS.
You and your partner sit down to grab a quick bite to eat when dispatch drops tones for a fall with injury. You arrive on scene and you find a 30-year-old male who has fallen approximately eight feet from a ladder. You find him in obvious distress and pain. You complete your primary survey, and you do not find any life threatening injuries. The patient denies any loss of consciousness, head, neck or back pain. Your patient has no known allergies or past medical history, a blood pressure of 162/90, heart rate of 112-sinus tachycardia, respiratory rate of 24, SpO2 of 99% on room air, and he rates his pain 10/10.
You expose the patient and complete your detailed trauma assessment where you find a closed tib/fib fracture to the right leg with pulses, motor movement and sensation present. You splint the extremity without issue, and you began transport to the closest appropriate facility that is at least 30 minutes away by ground. You decide to treat your patient’s pain, so you establish an IV and give the patient 100 micrograms of fentanyl with no adverse reactions noted.
Ten minutes after your medication administration, you notice that your patient is obtunded and difficult to rouse. You also note that the patient’s respiratory rate has dropped to nine, and his SpO2 is now 93% on room air. Would you start reaching for the Narcan? What if the same patient has received what you perceive as an adequate amount of pain medication, but he still rates his pain 10/10? His SpO2 reading is 93% on room air, and his respiratory rate is at 10? Are you comfortable giving him more medication?
EtCO2 Refresh
We have learned at all levels of EMS training that respiration is made up of both oxygenation and ventilation. We breathe in oxygen that gets carried to our cells for aerobic respiration, while CO2 is exhaled from the lungs as a waste product. SpO2 has long been relied upon as one of the cornerstone vital signs to determining the effectiveness of the patient’s respiratory status. With SpO2 alone however, we cannot assess the other part of respiration; and that is ventilation.
As EtCO2 monitoring has improved and become more readily available, EMS’ ability to assess ventilation and oxygenation has become much easier and accessible in the prehospital setting. EtCO2 monitoring is a tool paramedics can utilize in the field to confirm proper endotracheal tube placement, rule in/out differential diagnoses and monitor the effectiveness of respiratory medication interventions. Most importantly, measuring EtCO2 is the most accurate monitoring tool that paramedics can use in real time to assess the overall status of the patient in the field.
EtCO2 monitoring provides a capnography waveform that reflects the effectiveness of ventilation, as well as a capnometry reading that provides trending values estimating the amount of carbon dioxide that is exhaled with each breath. Normal EtCO2 is 35-45 mmHg and is broken down into four phases as noted in figure 1.

(Figure 1) A-B= Zeroed out baseline, B-C=Beginning of exhalation, C-D=Exhalation plateau, D=End-Tidal concentration that produces the numerical capnometry value, and D-E=Inspiration (Photo compliments to Dorchester County (SC) EMS for the use of their equipment.)
A normal EtCO2 waveform and capnometry value indicates that the patient is perfusing and breathing well through and unobstructed airway.1 What does this have to with pain management?
Literary Review
Appropriate pain management is vital part of patient care in the prehospital environment. Acute pain is the most common complaint presented to EMS providers with occurrence estimates ranging from 20 to 53%.2 As more EMS agencies expand their treatment options for acute pain management in the prehospital setting, the use of opiate pain medications – mainly fentanyl and morphine – have become more common.
Current evidence suggests that prehospital providers who adequately treat moderate to severe acute pain with appropriate doses of opiate pain medication prior to arrival at the emergency department will have a significant positive effect on the patient’s long term care and healthcare experience. Adequate pain management is crucial for EMS providers to achieve for several reasons. Adequate pain management helps to decrease patient anxiety, it helps to improve procedure success for painful interventions such as conscious IO placement, and it helps to facilitate movement and transport of the patient.
However, despite the widespread use of these medications, many EMS systems are failing when it comes to adequately treating and managing our patient’s pain in the field. Studies have shown that as much as 43% of our adult patients and 83% of our pediatric patients arrive at the ER without adequate pain management. Reasons for this shortfall include concerns for adverse reactions including nausea and vomiting, creating abnormal vital signs, with the most often cited concern being respiratory depression. Concerns were also raised that aggressive use of pre-hospital opiate pain medications would further add to the opioid abuse epidemic.2,3
As paramedics, we are well aware that opiate pain medications have the susceptibility to cause respiratory depression in our patients. We should not let this dissuade us from being good advocates for our patients when it pertains to treating their pain, when we can use EtCO2 to guide our care. Studies have demonstrated that continuous EtCO2 monitoring on patients undergoing procedural analgesia will detect incidences of respiratory depression far sooner than SpO2 alone.
Pooled data from three capnography studies showed that continuous capnography identified 8.6% more respiratory depression events versus pulse oximetry monitoring alone (CO2 group versus SpO2 group: 11.5% vs. 2.8%; P < .00001).4 One such study found that SpO2 monitoring only managed to identify 33% of patients that had an event of respiratory depression while EtCO2 found 100%.
McCarter, et al. demonstrated that EtCO2 monitoring was more beneficial at detecting respiratory depression events when compared to SpO2 monitoring and visual assessment alone by the patient’s healthcare providers. Of the 634 patients in the study that received opioid pain medication, nine had a respiratory depression event that required some form of intervention from the hospital staff. Four of the patients eventually received narcan. It is important to note that all nine patients were receiving supplemental oxygen during the respiratory depression event, and seven of the nine patients had a SpO2 reading greater than 92%.
In all nine patients, EtCO2 was the only parameter being monitored that alerted the staff to the respiratory depression.5 EtCO2 monitoring is the earliest and most reliable indicator of impeding respiratory compromise and can detect events of respiratory depression up to 271 seconds before changes are noted in the patient’s other vital signs. EtCO2 remains stable during movement and transport and produces accurate assessment information during states of poor perfusion.1 So how do we use all of this information?
Putting it Into Practice
We recommend that providers use EtCO2 monitoring on all patients receiving opiate pain medication prior to and in the course of the transport. If possible, patients should be kept in an upright position to avoid airway obstruction from the tongue. EtCO2 monitoring will produce a continuous real time waveform that will help to alert the provider of developing respiratory depression. This is noted by a prolonged waveform indicating bradypnea (see figure 2).
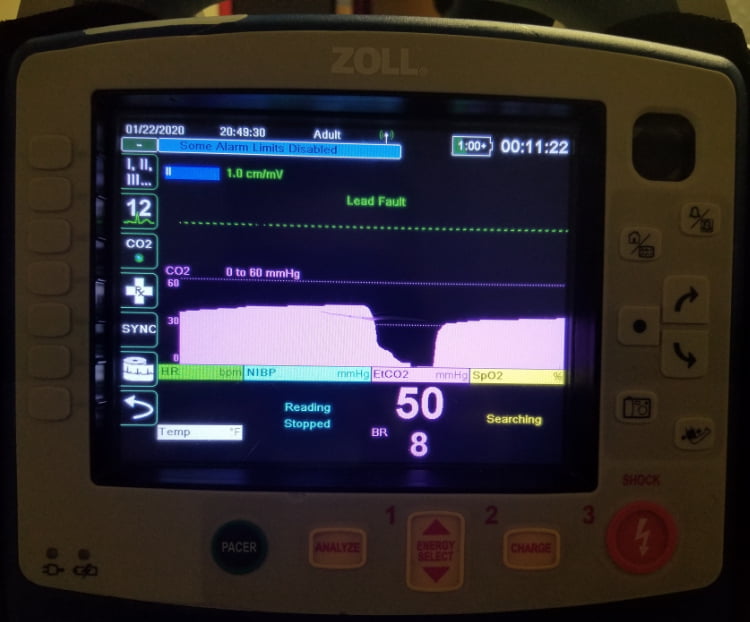
Figure 2. (Photo compliments of Dorchester County (SC) EMS for the use of their equipment.)
Providers should then begin to closely monitor and trend the patient’s capnometry values. Continuously rising capnometry values along with decreasing mental status, cyanosis and tachycardia could indicate that the patient is not ventilating well and is beginning to become hypoxic. The provider should then stimulate the patient to breath. If there is no noted improvement in the patient’s clinical presentation, the provider can consider the use of narcan titrated to the patient’s EtCO2 capnomtery value, mental status and vital signs with collaboration from an online medical control physician. Using EtCO2 monitoring as a guide, the provider can give smaller doses of narcan to treat the patient’s poor ventilation without completely reversing all of the patient’s analgesia or causing adverse side effects such as vomiting.
Case Resolution
You place your patient on an EtCO2 monitoring nasal cannula attached to supplemental oxygen at two liters per minute. You note a normal waveform and a capnometry value of 39 mmHg. Based on these findings, you administer an additional 50 micrograms of fentanyl. After 10 minutes you reassess your patient and find that his pain level is 6/10. You find him to still be ventilating well with an EtCO2 of 41 mmHg.
You are still 10 minutes away from the ER, so you continue with your pain management care and you administer an additional 50 micrograms of fentanyl. Upon arrival at the ER, your patient has a blood pressure of 110/78, heart rate of 92, respiratory rate of 14, SpO2 of 94% on supplemental oxygen, EtCO2 of 43 mmHg, and he rates his pain a tolerable 3/10.
Today’s EMS providers have more medications and lifesaving equipment available to them than ever before. As we continue to advance in the delivery of our medications and treatments, we need to ensure that we are providing the greatest benefit to each and every patient that we are called upon to serve. This task is best accomplished by wisely using every available piece of patient monitoring equipment to understand the whole picture of how your patient is doing. Using EtCO2 monitoring on every patient you administer pain medications to will give you the confidence to adequately and safely treat your patient’s pain, in addition to helping prevent and respond to adverse reactions in a timely manner.
References
1. Krauss, B., & Hess, D. R. (2007). Capnography for procedural sedation and analgesia in the emergency department. Annals of Emergency Medicine, 50(2), 172–181. doi: 10.1016. j.annemergmed.2006.10.016.
2. Diana M. Sobieraj, Brandon K. Martinez, Benjamin Miao, Mark X. Cicero, Richard A. Kamin, Adrian V. Hernandez, Craig I. Coleman & William L. Baker (2020) Comparative effectiveness of analgesics to reduce acute pain in the prehospital setting, Prehospital Emergency Care, 24:2, 163-174, doi: 10.1080/10903127.2019.1657213.
3. Friesgaard, K. D., Kirkegaard, H., Rasmussen, C.-H., Giebner, M., Christensen, E. F., & Nikolajsen, L. (2019). Prehospital intravenous fentanyl administered by ambulance personnel: a cluster-randomized comparison of two treatment protocols. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 27(1). doi: 10.1186/ s13049-019-0588-4.
4. Lam, T., Nagappa, M., Wong, J., Singh, M., Wong, D., & Chung, F. (2017). Continuous pulse oximetry and capnography monitoring for postoperative respiratory depression and adverse events. Anesthesia & Analgesia, 125(6), 2019–2029. doi: 10.1213/ ane.0000000000002557.
5. McCarter T, Shaik Z, Scarfo K, Thompson LJ. Capnography monitoring enhances safety of postoperative patient-controlled analgesia. Am Health Drug Benefits. 2008;1:28–35.
Thomas Krakeel, NRP, BS, is a paramedic crew chief and acting station supervisor for Dorchester County (SC) EMS.
Andrew Watson, NRP, BS, is a paramedic with Dorchester County (SC) EMS.




Game changer! This should change protocols for both prehospital and inpatient Conscious Sedation monitoring.