On the go? Listen to the article in the player below!
We all have it, some of us use it, but few use it to its full potential. I’m referring to the measurement of end-tidal carbon dioxide (ETCO2). The objective of this presentation is how to tell from those “expellings” the best way to optimize survival after cardiac arrest (CA). Our objectives will be to measure and use ETCO2, as an invaluable guide to resuscitation care.
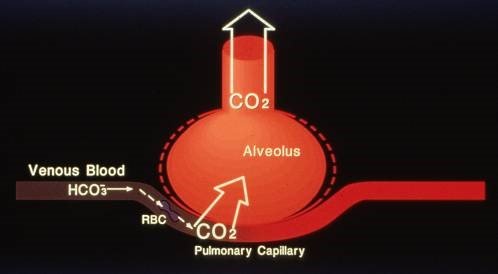
The concentration of CO2 in the air we breathe is 0.03%. Adults at rest produce approximately 2.5 mg/kg/min. This waste product of metabolism is then transported in one of two forms: in the blood or to the lungs, where it is cleared by alveolar ventilation. Sixty to 70 percent is converted by carbonic anhydrase and then bound to the bicarbonate ion. Twenty to 30 percent is bound to proteins (most available is hemoglobin). The final five to 10 percent is dissolved in physical solution, better known as the partial pressure of carbon dioxide (PaCO2); it is then exhaled through ventilation. The driving pressure for CO2 elimination is the partial pressure difference between the CO2 in the pulmonary capillary and the alveolar air. Equilibrium is reached in less than 0.5 seconds.
Exhaled CO2 is typically measured at the point of maximal exhalation, which is termed “end tidal” CO2. In some cases, measurement of total CO2 clearance is also of clinical value. ETCO2 can be displayed graphically and numerically. Numerically, it is called capnometry. Numerically and graphically, it is called capnography.
ETCO2 is usually measured by either mainstream, where the sensor and optical infrared sensor is in line with the inhalation/exhalation port of airway adjunct, or sidestream, where there is an aspiration device that transfers to the optical sensor.
ETCO2 is reported in different ways in various parts of the world. In North America, most reporting is in partial pressure or mm/Hg. It can also be reported in percentage, with one percent equaling 7.6 mm/Hg. In Europe and other countries, it is often reported in Kilopascal (kPa), with 1 kPa equaling 7.6 mm/Hg.
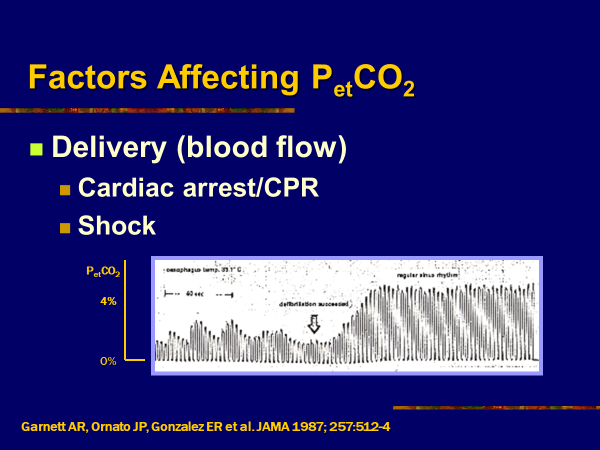
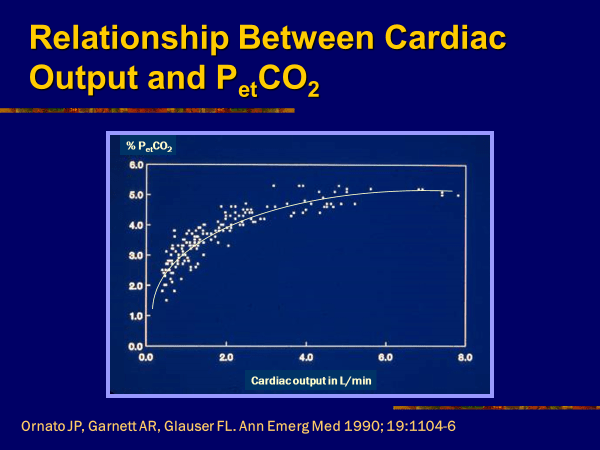
Factors affecting PaCO2 include delivery (blood flow) and elimination. Delivery is a reflection of cardiac output and is significantly affected by CA/cardiopulmonary resuscitation (CPR) and shock. A correlation between cardiac output and PaCO2 is shown below.
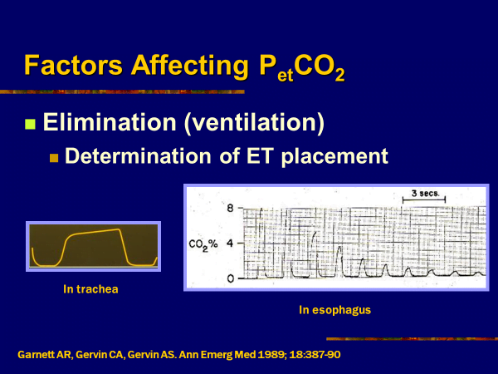
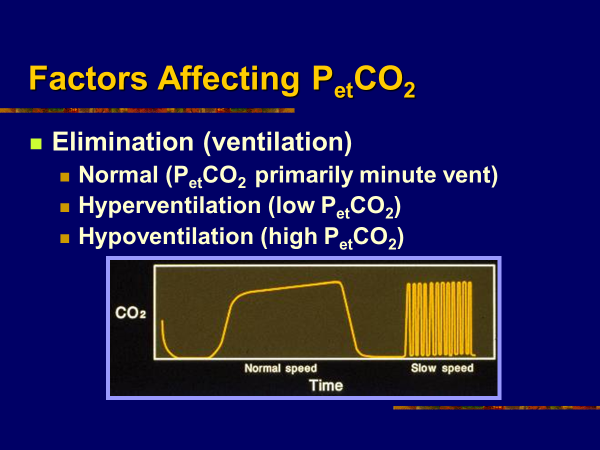
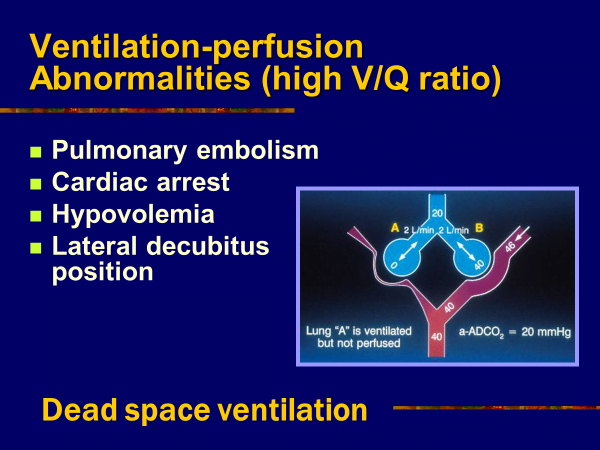
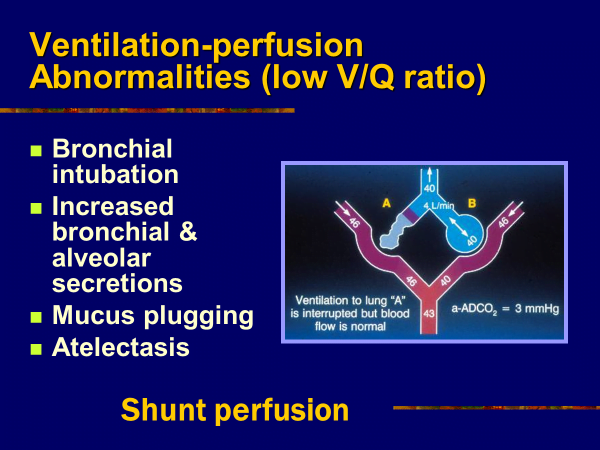
Elimination, on the other hand, is primarily a factor of ventilation, with results being directly and indirectly related to minute ventilation and tube placement. Examples are shown below.
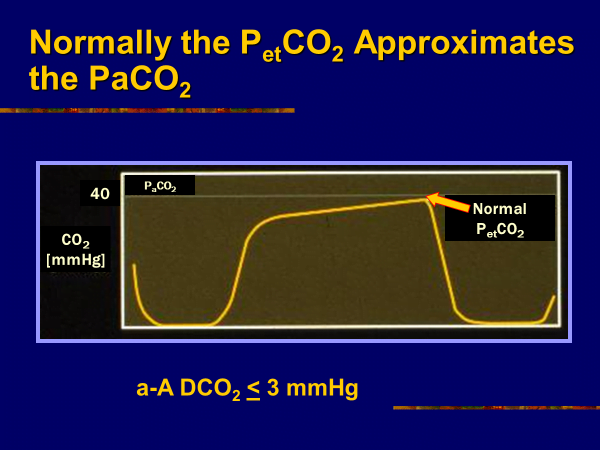
Although beyond the scope of emergency medical services, the relationship between PetCO2 (a reliable index of CO2 in PaCO2) and PaCO2 are important for evaluating ventilation and perfusion abnormalities. Normal a-ADCO2 (the difference between the arterial and alveolar ETCO2) is shown as well as ventilation/perfusion (V/Q) relationship.
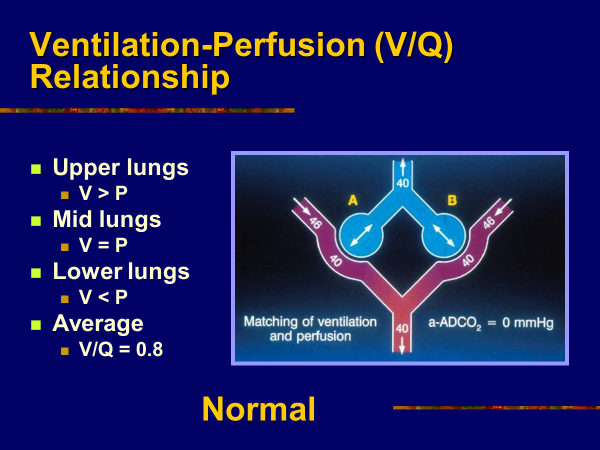
Although many factors affect a-ADCO2, and measuring these values many have limited prehospital use, in-hospital they are very valuable to determine both shunt and dead space ventilation. As noted, one relates to perfusion and the other to ventilation.
In addition, pre- and in-hospital values may be affected by a variety of diseases. These include asthma, chronic obstructive pulmonary disease, hyperventilation with incomplete emptying, and inadequate tidal volumes.
Clinical applications for prehospital care are primarily focused on tube placement or dislodgement, progress, or failure of resuscitation; in the non-arrested patient, it is focused on indications of obstructed airway disease.
It may also be useful to follow the progress of shock resuscitation in the nonarrested patient. One very important parameter is its use to follow the progress or failure of CA resuscitation. Studies we performed in the 1990s and which were published in the Annals of EM and the New England Journal of Medicine outline that potential and real use.
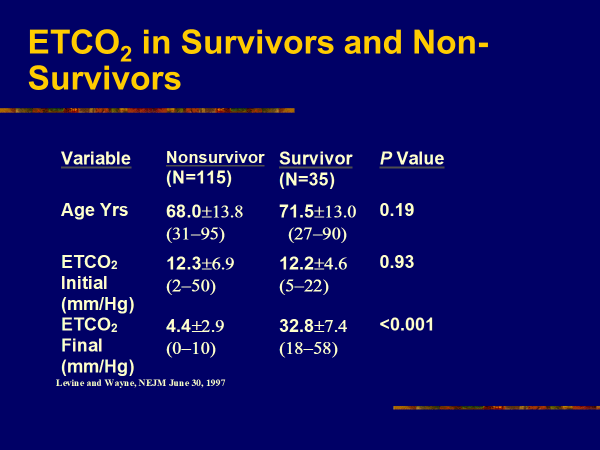
In the “real world,” the study was carried out for a total of 650 patients with consistent findings. Although study limitations are noted, the conclusions have impact for resuscitators and resuscitations. Limitations included patient numbers (see above), the effects of Epinephrine and Sodium Bicarbonate, and minute ventilation.
Best efforts were used to compensate and corollate for these effects. Our conclusions were that ETCO2 may be a marker of nonresuscibility, but it should not be used alone except with other parameters such as asystole to cease resuscitation. It should be noted that it is also is an excellent guide to progress of resuscitation, noting efficacy of CPR including rescuer fatigue. In combination with other devices such as ResQ CPR (cardio pump and POD) and/or mechanical CPR, head-up CPR may again show efficacy or failure of those devices. In the future, new technology and techniques may be evaluated by their effect on ETCO2.
ETCO2 may be a marker of resuscitation progress, with efforts to improve falling values such as changing rescuers for rescuer fatigue or shifting to mechanical devices. In combination with other parameters, it may be used to cease resuscitative care. Clearly, it is technically feasible and needs to be a significant part of both pre- and in-hospital care. There are obvious “Compelling Tellings from Expellings.”
Marvin A. Wayne, MD, FACEP, FAAEM, FAHA, is the medical program director for Whatcom County EMS systems in Washington state. He’s also an attending physician in the ED at St. Joseph Medical Center, an associate clinical professor in the Department of Emergency Medicine at the University of Washington, and is member of numerous local, state, national and international organizations on emergency medicine and EMS.