Ventilation strategies in prehospital care must balance pathology and physiology—especially in shock, where positive pressure ventilation can worsen outcomes if used without caution.
The general trend for ventilation strategies in the prehospital environment is that obstructive strategies are for patients with COPD and/or asthma and everything else gets put into the lung protective bucket.
These strategies are not new or even that novel now but became widely popular (and more palatable for the vent novice) with the help of FOAMed instructors like Dr. Scott Weingart (of emcrit) and Eric Bauer (of FlightBridge ED). This may be historically inaccurate, but they are how I was introduced to the topics.
Be it obstructive or protective, these ventilation strategies are both designed to protect the lungs from injurious settings while accounting for the (primary) lung pathology to allow for adequate ventilation and oxygenation. There are some universal elements that remain a constant issue regardless of the pathology or strategy chosen.
Things like plateau pressures (pPLAT), driving pressures, and new to the list is mechanical vent power are all ways that clinicians look at the force of ventilation and how it is affecting the lung tissue. When boiled down to the bare elements the goal is to avoid:
- hypo/hyper-ventilation
- hypoxia / hyperoxia
- alveolar damage leading to the development of ARDS
But there is the flaw in that logic. Just using a lung protective strategy alone does not prevent ARDS. Cardiac arrest, shock and trauma are direct causes of ARDS in and of themselves as well as ventilator induced lung injury (VILI). The point is the damage is done in some cases. The goal is then to attempt to slow the advancement and severity of ARDS.
Mechanical ventilation is simple: oxygenate, ventilate, and do not injure the lungs while doing so. There are only two pathways to worry about and if the patient does not have a primary obstructive physiology, we know what we are going to do… right?
Welcome to the equation: the hemodynamically unstable patient. There is one very necessary intervention in the shocked patient that, if done carelessly, will absolutely make the situation worse.
Not worse like running out of hot water in the shower on a cold day. Worse like a fire truck pumping gasoline through the hose line on a structure fire.
That intervention is positive pressure ventilation (PPV).
The Problem of Positive Pressure Ventilation
The combination of shock physiology, hypotension and positive pressure ventilation may be one of the most dangerous, yet underappreciated physiologic combinations encountered by prehospital clinicians.
So dangerous that this combination should be avoided, whenever possible, by allowing the patient to protect their own airway and ventilate on their own. As we all know, this is not always practical or possible.
Sometimes the patient is exceedingly sick and requires airway management and ventilation to achieve adequate minute ventilation and oxygenation goals in the presence of shock and hypotension.
How does this cause problems?
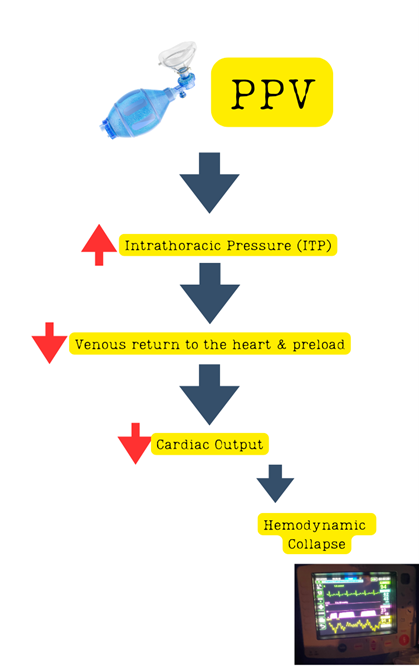
Image created by the author.
PPV causes increased intrathoracic pressure (ITP). High ITP causes decreased venous return to the heart and preload. A reduction in volume returning to the heart (preload) means that there will be reduced cardiac output. Unless we correct this, it will eventually lead to hemodynamic collapse.
These patients are exceedingly sick. So much so that “blanket” strategies require some significant modification. There are multiple competing priorities and even small adjustments of some interventions can increase the problems downstream. In this case, a “hypotensive vent strategy” or “hemodynamically neutral strategy” is necessary.
Hemodynamically Neutral Ventilation
What it is a hypotensive or hemodynamically neutral ventilation strategy? It is a simple modification of the elements of minute ventilation that still achieves the goals of adequate minute ventilation and lung protection.
This type of ventilation strategy has been studied in the cardiac arrest population as well as the post arrest/ROSC population as well, and it is that research that informs this approach in the CCT environment.1 Clinicians must be patient with this strategy and give the patient time to respond to the treatments.
These patients have a primary hemodynamic instability problem, not a primary lung pathology problem. Meaning, the ventilator needs to be set up to ensure adequate minute ventilation and oxygenation, but it is not the primary instrument that is going to be used to stabilize the patient.
Clinicians need to ensure that it does not get in the way of the resuscitation and steal the show from the hemodynamics. In fact, it can be set up to support those hemodynamics instead of endangering them.
The protocol is simple:
- Larger tidal volume (8cc/kg IBW) instead of a “standard” 6cc/kg IBW
- Slower respiratory rate (12-14/min).2,6
(Note: ensure the proper minute ventilation is targeted and is met during care).
- PEEP is started lower (5-8) and carefully titrated with close attention paid to the hemodynamic situation.
The benefits are many:3
1.) Lower alveolar pressures (pPLAT <30 is the target) –> lower risk of ARDS development.
2.) Lower intrathoracic pressure –> improved hemodynamics.
3.) Lower driving pressure –> reduced alveolar pressure and lower risk of ARDS development.
4.) Lower mechanical ventilator power –> less lung strain and therefore less inflammation à lower risk of ARDS.
5.) Lower rates –> reduced dead space ventilation which encourages better CO2 management.1,4-5
The risks require close attention:
In the shocked patient, there are some competing priorities. Metabolic acidosis is usually present and the primary method for compensation is increased minute ventilation. But careless titration of respiratory rates up to achieve this can further complicate the clinical picture.
If done carelessly, it can do more harm. It is much more effective to target the cause of the acidosis and work to correct that issue rather than target the acidosis itself (the deeper discussion is a topic for another day).
PEEP presents an interesting challenge as it is vital for the recruitment of and maximization of alveolar surface area. It is also a crucial part of managing the driving pressure, which is a function of PEEP and pPLAT (driving pressure = pPLAT – PEEP).3 The clinician must balance the need to increase PEEP with the overall hemodynamic situation.
There will be a time for higher PEEP, but in the presence of hemodynamic instability that is labile or unresponsive to aggressive pressor support it is best to take a slow and judicious approach to increasing PEEP beyond certain thresholds. The literature, predictably, cannot agree on what that number may be.
Beware of letting the ventilator steal the show. Chasing a low SPo2 in a patient in shock with PEEP titrations will invariably land the patient in bad situation. Focus instead on forward flow and cardiac output to increase SPo2 readings (it is perfusion dependent after all). Once a reasonable MAP has been obtained and stabilized, it is then prudent to begin to manipulate PEEP to improve oxygenation and alveolar recruitment.
Close Out
The adage of “you can never have too much of a good thing” is regularly challenged in medicine. The hemodynamically unstable patient that requires mechanical ventilatory support is no exception.
The critically ill often confront clinicians with situations in which the patient is in extremis with multiple competing priorities. How those elements are prioritized and addressed can positively or negatively impact the patient’s situation. Sometimes modifications from “the norm” are required, and they do exist with good evidentiary support.
Hemodynamically intrusive vent settings, to borrow the phrase from Davis et al, may make some of the physiologic measure “look better” but the underlying physiology is getting worse and will assuredly greatly complicate the course of care.
A simple protocol of “easy” ventilation with a larger breath at a slower rate just may give the clinicians the time and protection they need to move the patient’s physiologic predicament forward.
References
- Lazzarin T, Tonon CR, Martins D. Post-Cardiac Arrest: Mechanisms, Management, and Future Perspectives. J Clin Med. 2022 Dec 29;12(1):259. doi: 10.3390/jcm12010259. PMID: 36615059; PMCID: PMC9820907.
- Daniel P. Davis, Paul W. Davis, A structural model of perfusion and oxygenation in low-flow states, Resuscitation, Volume 82, Issue 11, 2011, Pages 1444-1452, ISSN 0300-9572, https://doi.org/10.1016/j.resuscitation.2011.05.028
- Robba C, Badenes R, Battaglini D; TTM2 Trial Collaborators. Ventilatory settings in the initial 72 h and their association with outcome in out-of-hospital cardiac arrest patients: a preplanned secondary analysis of the targeted hypothermia versus targeted normothermia after out-of-hospital cardiac arrest (TTM2) trial. Intensive Care Med. 2022 Aug;48(8):1024-1038. doi: 10.1007/s00134-022-06756-4. Epub 2022 Jul 2. PMID: 35780195; PMCID: PMC9304050.
- Aufderheide TP, Sigurdsson G, Pirrallo RG. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004 Apr 27;109(16):1960-5. doi: 10.1161/01.CIR.0000126594.79136.61. Epub 2004 Apr 5. PMID: 15066941.
- Katzenschlager S, Popp E, Wnent J. Developments in Post-Resuscitation Care for Out-of-Hospital Cardiac Arrests in Adults-A Narrative Review. J Clin Med. 2023 Apr 20;12(8):3009. doi: 10.3390/jcm12083009. PMID: 37109345; PMCID: PMC10143439.
- Marchese G, Bungaro E, Magliocca A. Acute Lung Injury after Cardiopulmonary Resuscitation: A Narrative Review. J Clin Med. 2024 Apr 24;13(9):2498. doi: 10.3390/jcm13092498. PMID: 38731027; PMCID: PMC11084269.
Cody Winniford is a flight paramedic and base manager in Baltimore, MD. He has a passion for sharing his professional experience in EMS and management. Cody’s clinical and leadership development background spans both military and civilian settings and has served in several capacities as a leader and prehospital clinician. He specializes in air medical and critical care transport, as well as organizational development and leadership development. He is an active speaker on various leadership and clinical topics and is an established and successful educator for prehospital clinicians of all levels. He has a passion for human performance improvement and the mental health and performance aspects of prehospital care.


