On the go? Listen to the podcast below!
Airway management in the prehospital environment is difficult just by virtue of where we are doing it and the lack of resources available to help us manage the difficulties. Add to that a patient with mangled facial anatomy or is dangerously peri-arrest due to hemorrhage and the danger can seem insurmountable.
What the research tells us is that there are really three big buckets of problems in airway management that contribute to morbidity and mortality: hypoxia, hypotension and multiple intubation attempts; this is the stuff that airway nightmares are made of. This small chunk of airway literature gives us valuable insight into the danger:
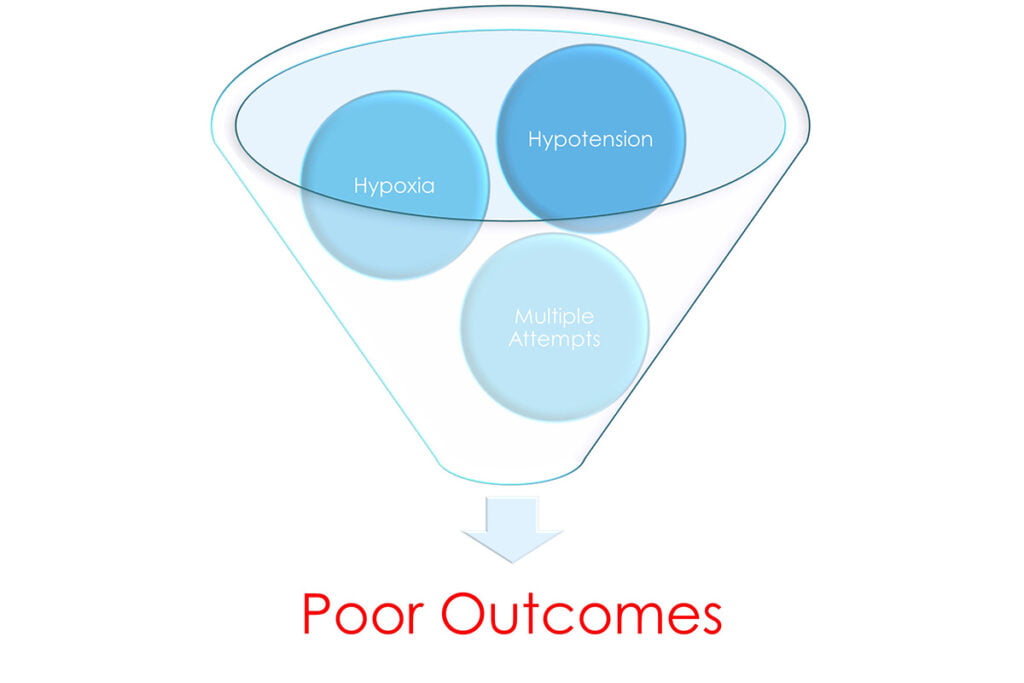
Image created by the author.
- Hasegawa, K. (2012). Association Between Repeated Intubation Attempts and Adverse Events in Emergency Departments: An Analysis of a Multicenter Prospective Observational Study. Annals of Emergency Medicine , 749-754.
- Heffner, A. (2012). Predictors of the Complication of Postintubation Hypotension During Emergency Airway Management. Journal of Critical Care, 587-593.
- Heffner, A. (2012). The frequency and significance of postintubation hypotension during emergency airway management. Journal of Critical Care, 417-419.
- Jarrod M. Mosier, M. J. (2015). The Physiologically Difficult Airway. West J Emerg. Med., 1109-1117.
- Sackles, J. (2013). The Importance of First Pass Success When Performing Orotracheal Intubation in the Emergency Department. Acad Emerg. Med., 71-78.
- Weingart, S. (2012). Preoxygenation and Prevention of Desaturation During Emergency Airway Management. Annals of Emergency Medicine, 165-175
This is a little over 5,000 patients and outcomes that tell us that we should work very hard to approach airway management (in general) very carefully.
What does good airway management look like in a trauma patient?
- Got the tube no matter how many attempts or adverse events?
- Got it on the first attempt, the patient de-satted, and they recovered?
- Got it on the first attempt, no desaturation, but hypotensive after placement?
- Got it on the first attempt, no desaturation, no hypotension?
- Got it on the second attempt, no desat, no hypotension?
- Any adjunct placed on first attempt w/out desat, hypotension?
It actually comes down to three simple metrics: first pass success without hypoxia or hypotension. This is commonly referred to as DASH-1A (definitive airway sans hypoxia and hypotension on the first attempt, thanks to Bill Hinkley MD for this one).
In some cases, particularly in trauma, this is not always possible or attainable. Trauma patients often present hypoxic and hypotensive, and sometimes with mangled airway anatomy that makes intubation difficult if not impossible.
Difficult Airway Management
All airways are difficult to some degree. Part of mitigating that difficulty is clearly identifying why it is difficult in the first place. The overarching issue is failing to properly assess for difficulty and adjust the approach to better suit the patient. Any one of these predicted difficulties can lead to one of the aforementioned contributors of airway morbidity and mortality (hypoxia, hypotension, and multiple attempts).
Specifically, we are looking for one of the following issues:
- Difficulty with obtaining a view and placing a tube.
- Difficulty with secondary/rescue device placement and utilization (BVM/SGA/Cric)
- Apnea intolerance (due to physiologic derangement)
- Hypotension/Hemodynamic Instability
- Contextual/Situational Issues
These can be further classified into one of two “difficult airway” buckets: physically and physiologically difficult airways.
Traumatized and Physically Difficult Airways
Physically difficult airways are those that present with either a difficulty in visualizing the glottic opening, physically placing a tube, or instrumenting the airway. Other difficulties such as not being able to obtain and maintain a BVM mask seal, poor neck mobility, and massive amounts of emesis or bleeding in the oropharynx can also contribute to the physical difficulty of securing the airway.
Within the context of trauma, the airway anatomy can be damaged and/or distorted to the degree that simply identifying landmarks can be incredibly difficult. This is often complicated by the presence of copious amounts of blood in the oropharynx that can make it even more difficult to visualize the glottic opening and pass the tube.
Physiologically Difficult Airway Management in Trauma
Physiologically difficult airways present us with a set of challenges where our ability to address or correct hypoxia and/or hypotension is limited. There may also be other physiologic factors that make the procedure even more dangerous (like a metabolic acidosis). The danger with these types of issues is that the patient does not have enough (or any at all) physiologic reserve to be able to tolerate the apnea period after paralysis in RSI and may not be able to tolerate the procedure without a deliberate period of resuscitation prior to induction.
Hypotension is the most dangerous issue paramedics can encounter in these situations as it is the number one predictor of post intubation cardiac arrest. In trauma it is difficult to control, and hypotension (permissive hypotension specifically) is an element of trauma resuscitation. Add to all of that the need to ventilate the patient with positive pressure (either before or after tube placement) can exacerbate any hypotension that may be present.
Pre-Planning and Responses
The key and essential element of trauma airway management is pre-planning the procedure to address the known and anticipated difficulties that may be encountered. We have a plethora of tools at our disposal to mitigate the issues associated with physically and physiologically difficult airways and it is important that those tools are organized into a system of responses to the difficulties encountered.
One system of contingency planning that I have presented in the past is the PACE planning system. With its origins in the military special operations community, PACE planning allows for a clinician to pre-plan responses to encountered difficulty in airway management.
P – Primary: this is the plan A, standard approach that would be utilized if there was no encountered difficulty.
A – Alternate: this is your plan B, which is just as effective as plan A, but required some minor modification in order to execute the plan safely.
C – Contingency: this is what you would use if you had to completely bail out on the desired approach (think abandoning intubation altogether), yet still effectively manage the airway with this approach.
E – Emergency: this is the last resort, “bail out” situation that in most systems is built around surgical front of neck access (FONA).
The great thing about this system is that it allows for the situation to develop and for the clinicians at the bedside to respond to encountered difficulties without having to go back to the drawing board each time there is a “failure.” It protects the clinician’s mindset and cognitive function by allowing them to “fail forward” by having a plan in place for when things go wrong.
There is a difference between failing to plan for problems and planning to fail. By planning to fail, the clinician acknowledges that there is a good chance that Plan A will not work out and they need to have some back-up plans.
By failing to plan, however, the clinician will likely not have a preplanned response to problems, quite possibly to the patient’s detriment.
Cody Winniford is a flight paramedic and base manager in Baltimore, MD. He has a passion for sharing his professional experience in EMS and management. Cody’s clinical and leadership development background spans both military and civilian settings and has served in several capacities as a leader and prehospital clinician. He specializes in air medical and critical care transport, as well as organizational development and leadership development. He is an active speaker on various leadership and clinical topics and is an established and successful educator for prehospital clinicians of all levels. He has a passion for human performance improvement and the mental health and performance aspects of prehospital care.


