1. Introduction
Simulation-based training (SBT) has been utilized by many allied healthcare professions (AHPs), such as paramedics and emergency medical technicians (EMTs). Airway management, including – but not limited to – Endotracheal Intubation (ETI), is a lifesaving component, which might be required in some prehospital settings, such as cardiopulmonary resuscitation (CPR), trauma management, and other medical emergencies. Although the SBT is an essential measure of clinical competency for paramedics and EMTs, there is still a knowledge gap in the proper design of SBT programs and their impact on ETI skill retention in clinical practice.1 This project aims to develop an ETI-SBT-On-the-Go program for continuing professional development (CPD) to be accredited by the Saudi Commission for Health Specialties (SCFHS) to assess and enhance the ETI skill retention of paramedics at the workplace.
2. Problem Identification
According to the Department of Health and Social Care: Paramedics are highly trained healthcare professionals capable of responding to patient needs.2 However, this broad scope of their practice could cause some issues due to the infrequent nature of some cases.3 Risk of skills decay in rarely performed events, such as ETI.4 Training programs are essential to maintain paramedics’ competency in performing airway management, including ETI. It was unclear in the literature which program design could help to maintain skills retention. The ETI skill decay occurred within six months of training and two years post-training.5
3. Problem Significance
Unsuccessful attempts of the ETI along with several pathological conditions might affect brain perfusion and oxygenation and cause brain anoxic injury which leads to increased mortality and morbidity rates among patients.6 Using the right equipment and training programs could enhance the intubation-related skills of paramedics and mortality and morbidity outcomes. In out-of-hospital settings, ETI is a mandatory skill required by well-trained paramedics. The Paramedics and EMTs rely more on SBT than other AHPs. The educational level (period) of EMTs is a limitation point. During COVID-19, the Committee on Accreditation of Educational Programs for the Emergency Medical Services Professions (CoAEMSP) and the Commission on Accreditation of Allied Health Education Programs (CAAHEP) rectified their standards and reinforced the use of the SBT, respectively.
4. Previous Attempts
Although pre-hospital ETI has been proven to help control ventilation and secure the airway, the decay of ETI skills amongst paramedics and its adverse effects on patients’ lives were observed. A literature review of all relevant studies was conducted to overview the impact of skill retention on endotracheal intubation in out-of-hospital settings. The study review of Pilbery (2018) evaluated the literature from the 1970s when the role of paramedics started and was focused on how paramedics (eligible or inclusion criteria) and emergency medical technicians (EMTs) learn and maintain endotracheal intubation (ETI) skills. They found that there was no clear evidence to measure and maintain paramedics’ ETI skills (no specific benchmark). A range of measures was suggested to assess competency-related intubation skills in out-of-hospital settings, such as intubation success and complication rates, laryngoscopy technique, and decision-making. Furthermore, an annual Intubation training program on multiple types of airway manikins was proposed to be designed and supervised by experienced faculty members. Limited opportunities for paramedics to practice and maintain intubation-related skills clinically left the research question of this study unanswered, and thus further research is needed to elucidate how paramedics maintain their ETI skills in out-of-hospital settings.8
According to the European Resuscitation Committee (ERC) guidelines (2015), the medical staff performing intubation during cardiac arrest should be part of a monitored program (including a regular competency-based training program to maintain their skills). Another study was conducted to develop an SBT program on ETI for pre-hospital paramedics using Airtraq and evaluate the outcome of the obtained skills in out-of-hospital cardiac arrest (OHCA) patients. The paramedics involved in this study had no previous experience with intubation. Although the ETI with Airtraq can be learned with a simple SBT program using different airway trainers and can be performed safely when dealing with real cardiac arrest patients. Moreover, regular updates and recertification could help to maintain the retention of skills. Unfortunately, the study recorded a low success rate with failed intubation attempts using the Airtraq due to laryngoscope aspiration and airway secretion comparable to other studies. Thus, it was recommended that more control is required to maintain and safely transfer skills from SBT to clinical practice.9
Most of the previous studies demonstrated that paramedics have deficiencies in their intubation skills with high-risk, low-frequency pediatric cases in out-of-hospital settings. A recent study conducted by Lammers et al. (2022) included full- and part-timer paramedics who completed the Pediatric Education for Prehospital Professionals (PEPP) course six to eight months before the study. The study included five agencies from different regions and was geographically separated to cover diverse populations. Clinical Assessment Modules (CAMs) simulations were conducted in a standardized manner, and real-time scoring was used for observation and correction. According to the study design and educational interventions, participants were randomly divided into four groups: high-fidelity simulation training (HFSim), low-fidelity simulation training (LFSim), lecture and procedure skills lab training (LPSL), and standard, online pediatric refresher course (Control). The results of this study revealed that LFSim using a range of difficulties in scenarios, tools, and multiple learning strategies, was adequate for teaching pediatric intubation skills to paramedics compared to HFSim and online refresher courses. Moreover, measuring the rate of degradation of the related skills will help to set an interval schedule of refresher training programs sufficient to produce a substantial improvement and rarely maintain practice skills.10
An additional research study was conducted on pre-hospital airway management training and education. The duration and frequency of training required to attain competency in pediatric skills are unknown. It was found that within six months of training, emergency medical services (EMS) clinicians exhibited greater skill decay with ETI and more pronounced in a period of two years after training which is in close accord with the observations reported by Lammers and his colleagues in the management of pediatric emergencies using four different methods of paramedic continuing education.10 Thus, sustainable periodic competency evaluations for the EMS training programs must be integrated and supported by quality management programs to maintain an acceptable level of EMS clinicians’ competency in knowledge and skills. These results are agreed with the recommendations of the National Association of Emergency Medical Services Physicians (NAEMSP).11
Airway management is an active engagement in deliberate practice for lifesaving. Dorset et al. (2022) reported that one intubation per quarter was enough to demonstrate continued competence in difficult airway intubations. The related training programs and activities must cover all competency aspects (Knowledge, Skills, and Attitude; KSA) as goal-oriented practice and a well-defined task to improve performance over time. Thus, the training program should be designed according to the participant’s level with detailed instructions, opportunities for repetition, and immediate feedback on their performance for corrective action and improvement plans. Based on the NAEMSP, credentialing, and CPD activities in airway management are essential to obtain and maintain the level of clinicians beyond entry-level competency and upon patient-related needs.12
5. Proposed Solution
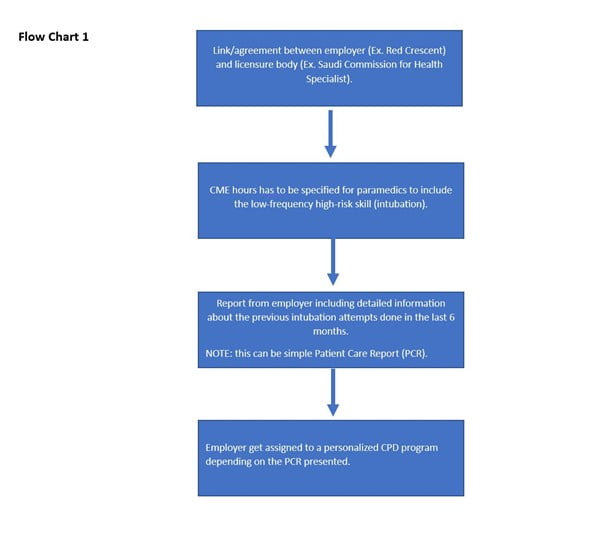
The included literature review in this project suggests that having a periodic continuing education program is important to maintain the intubation skills of paramedics. These programs must include in-person practical skills sessions, not online.10 As suggested by Nørregaard, Annette and others,9, 11 these CPD programs should be integrated and supported by a quality management (recertification) program. Locally we can refer to the Saudi Commission for Health Specialists (SCFHS), which can mandate specific CME hours for paramedics to include prehospital intubation skills. This can be done through a collaboration between the employer (Ex. Saudi Red Crescent Authority; SRCA) and SCHS. According to the literature analysis, the specific time for the intubation skill decay was unclear, but8 suggested having an annual intubation training program. To satisfy this, the employer at the end of the year will send a report including the previous intubations done by each paramedic so he/she can provide it to SCHS for the completion of the CME hours required for recertification. This report will include the attempts’ details in the Patient Care Report. Using this PCR, the paramedic will be assigned a personalized CPD program depending on the previous intubation attempts, as suggested by Lammers and Dorsett.10, 12 See Flow Chart 1.
Flowchart 1: for the SBT Program.
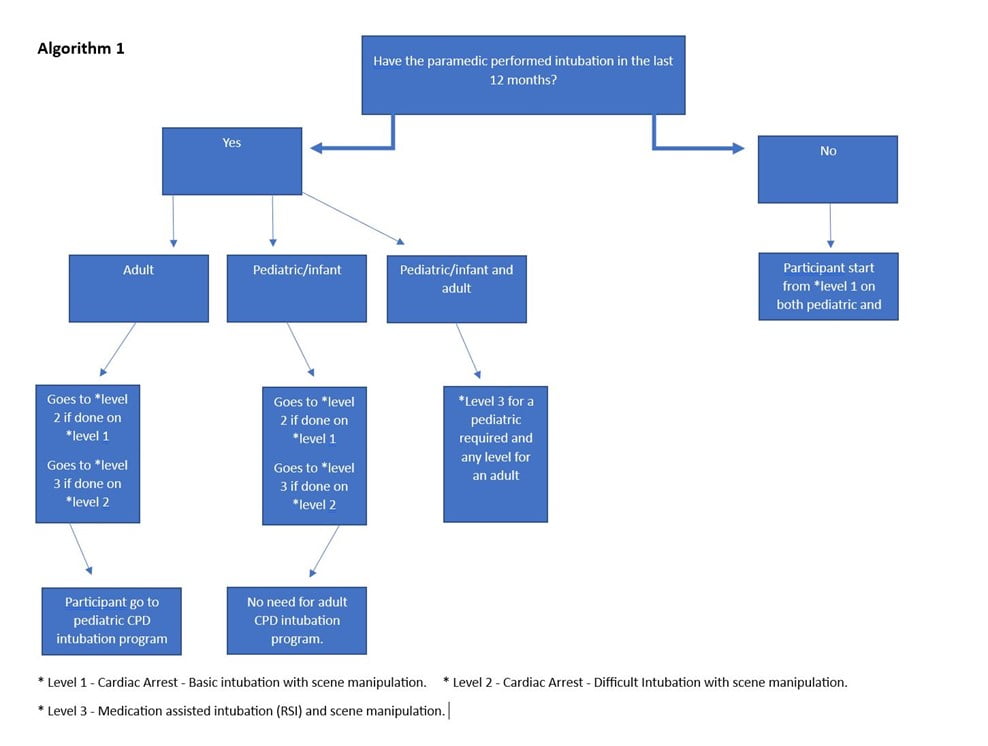
To create a personalized educational experience depending on the level of the paramedic, Algorithm 1 was created. In that, three levels of prehospital intubations were included. Scene manipulation was added to all levels as the prehospital environment requires different settings to increase the fidelity of the training. The difficulty of the scenes or environments could be adjusted accordingly.
Level 1 Cardiac arrest – Basic intubation with scene manipulation.
Basic intubation means that the patient does not have any airway difficulties based on the 3-3-2 airway rule.
Level 2 Cardiac arrest – Difficult intubation with scene manipulation.
Difficult intubation could include a Mallampati score of three or four, short neck, obesity, or any other features identified by the senior instructor.
Level 3 Medication assisted intubation (RSI) with scene manipulation.
This level includes medication calculation and administration to sedate and paralyze the patient before intubation.
Those three levels will help in the placement of the paramedic before enrolling in the CPD program. The PCR forms should indicate the details of the intubation attempts done by the paramedic and under which circumstances. Then the instructor should be able to check which of the three levels the paramedic satisfied. if the paramedic has done only 1 intubation on an adult patient with no complications in the scene or the features of the patient, then the paramedic will be placed in level 2 (adult) as he/she has already completed level 1 for adults but still needs to satisfy the pediatric side of this level. The CPD program following this algorithm and using the PCRs for each paramedic will create a unique experience according to the level of the paramedic. The PCRs will be used to help the instructor recreate the failed intubation attempts or successful but needs improvements in a simulated environment. As explained in Dorsett (2022),12 active engagement in deliberate practice should be the guiding approach for developing and maintaining competence in airway management. This includes, “Learners must have ample opportunities to improve their performance by performing the same or similar tasks repeatedly.”
Alorithm 1: SBT Program.
6. Simulation Tool
According to the literature,10 high-fidelity simulators were not needed when used during cardiac arrest scenarios and low fidelity was sufficient with instructive scenarios and a good debriefing session. Partial task trainers or low-fidelity manikins with specific features will be lower in cost. Prehospital intubations are different from intubations done in the emergency room (ER) or operation room (OR). Thus, the simulation environment should mimic those special circumstances, see Table 1.
Table 1. Simulation Resources.
| Simulation environment | Three separate rooms to accommodate the three different levels.
– Level 1 room: have airway task trainers’ adult/pediatric with all the equipment needed for the intubation. The scene manipulation will depend on the scenario and can be imaginary (open for the instructor’s creativity ex. use a distractor like an agitated family member). – Level 2 room: has all the previous features, but different airway manikins with difficult features adult/pediatric. Ex. Small mouth opening, short neck, etc.) – Level 3 room: have all the previous features plus, medications and all necessary equipment to perform the RSI intubations. Note: To increase the realism of the scenario we recommend having an ambulance model equipped with a stretcher and all features of the ambulance cabin. A full-body manikin can be used in this case. |
| Technology Resources | Video recording can be an added feature but not necessary. Recording can assist in the debriefing session as recommended by one of the studies.20 |
7. Simulation Tool Intervention
The program is based on the standards of the International Nursing Association for Clinical Simulation and Learning (INACSL-2021). Their framework included eleven criteria for developing effective simulation-based experiences.13
Criterion 1: Designer/simulationist expertise in simulation-based education.
This is an updated criterion added to the 2021 standards, which emphasizes the importance of training instructors to be effective simulators. This requirement can be met through several methods, including – but not limited to – certification in medical education.
Criterion 2: Needs assessment.
In addition to the needs assessment discussed above, the existing licensure requirement for paramedic recertification does not satisfy this skill gap. Those courses include (PALS, ACLS, PHTLS, and CME hours).10 In addition, the SCFHS does not have any practical CPD sessions for airway management.
Criterion 3: Measurable objectives.
A table was developed including the objectives with alignments to the three levels as shown in Table 2. The broad objectives for this program are:
- Ensure the maintenance of intubation skills of adults and pediatrics by evaluating the paramedic’s PCRs in the last 12 months if intubation was attempted.
- Evaluate the current paramedic skills of intubation by enrolling him/her in simulation-based training.
Table 2. Alignment of levels and objectives.
| Those levels apply to both pediatric and adult intubations. | Objectives | |
| Level 1 | Cardiac Arrest – Basic intubation with scene manipulation | To achieve the precision level in the psychomotor domain:
– Accurately perform the intubation on an adult/pediatric manikin choosing the right sizes and equipment. – Control the scene proficiently while performing the intubation. |
| Level 2 | Cardiac Arrest – Difficult Intubation with scene manipulation | To achieve the articulation level in the psychomotor domain:
– Control the scene proficiently while performing the intubation. – Integrate the manipulation of a difficult airway (Ex. positioning, using a bougie, etc.) while performing the intubation. – Perform the intubation in a timely manner without interrupting the compressions for more than 5 secs. |
| Level 3 | Medication assisted intubation (RSI) and scene manipulation | To achieve the naturalization level in the psychomotor domain:
– Control the scene proficiently while performing the intubation. – Automatically recognize the need for the use of medications to perform intubation. – Calculate the doses of medications with perfection. – Perform the intubation on an adult/pediatric with perfection. – Perform all steps of the intubation in a timely manner (RSI medication administration, preoxygenation, intubation). |
| *Basic intubation: Direct endotracheal intubation on a regular manikin.
*Difficult intubation: Direct endotracheal intubation with difficult airway features (Ex. Small mouth opening, large tongue, etc.) *RSI intubation: Using a sedative and a paralytic to perform the intubation. |
||
Criterion 4: Alignment of simulation modality and objectives.
The modality of this simulation-based training is a procedural simulation using partial task trainers/full body manikins (adult/paediatrics) with ranges of difficulty this can include internal or external features. According to Lyng,11 high-fidelity simulators were not needed for teaching pediatric resuscitation skills. For this program, low fidelity and partial task trainers should satisfy the objectives intended with the lowest cost.
Criterion 5: Scenario design.
The scenarios should be scripted and built to achieve the objectives of the level intended for, can refer to Table 2:
- Each scenario should start with measurable objectives aligned to the correct level.
- Realistic background situation, preferably from a real experience by the instructor or recreation from the PCR.
- Brief and focused on airway management which ultimately leads to intubation.
- Arranged by levels to ensure easier categorization and later use.
- Specific to the different complications/differences between adult intubations and pediatric intubations.
- Each scenario should include critical failure points/actions as shown in the Out of Hospital Skill Sheet (Appendix).
- The time frames of each scenario should be reasonable to achieve the objectives.
Criterion 6: Use of various fidelity
For this program different types of fidelity are not needed rather, scene manipulation, full-body manikins, and an ambulance model should be used to increase and mimic the out-of-hospital challenges with intubations and increase the realism of the scenario.
Criterion 7: Learner-centered approach
This personalized CPD program driven by specific objectives for each level, depending on each paramedic’s previous attempts will ensure a facilitative learner-centred approach. The facilitator plays a key role in determining the appropriate level of involvement following the learner’s level. The facilitator or instructor should keep in mind the diversity of cultures and values of learners.
Criterion 8: Prebriefing
The prebriefing plan and materials should be written for each scenario/case to be used as a guide and include:
- Learning objectives developed in accordance to and level.
- Identification of participants’ expectations, ground roles, and logistics.
- Establishment of psychological safety.
- Orientation of space, equipment, simulator, method of evaluation, etc.
Criterion 9: Debriefing/ feedback
Since this program closely relates to life support courses provided by the American Heart Association (AHA), their debriefing method; Gather, Analyze, and Summarize (GAS) has been adopted to maintain consistency for the instructor and learner.19 Depending on the level of the scenario, debriefing and/or feedback can be used. A simple case intubation scenario (Ex. level 1) can be followed by feedback only and a more difficult scenario (Ex. level 2&3) should be followed by a debriefing session.
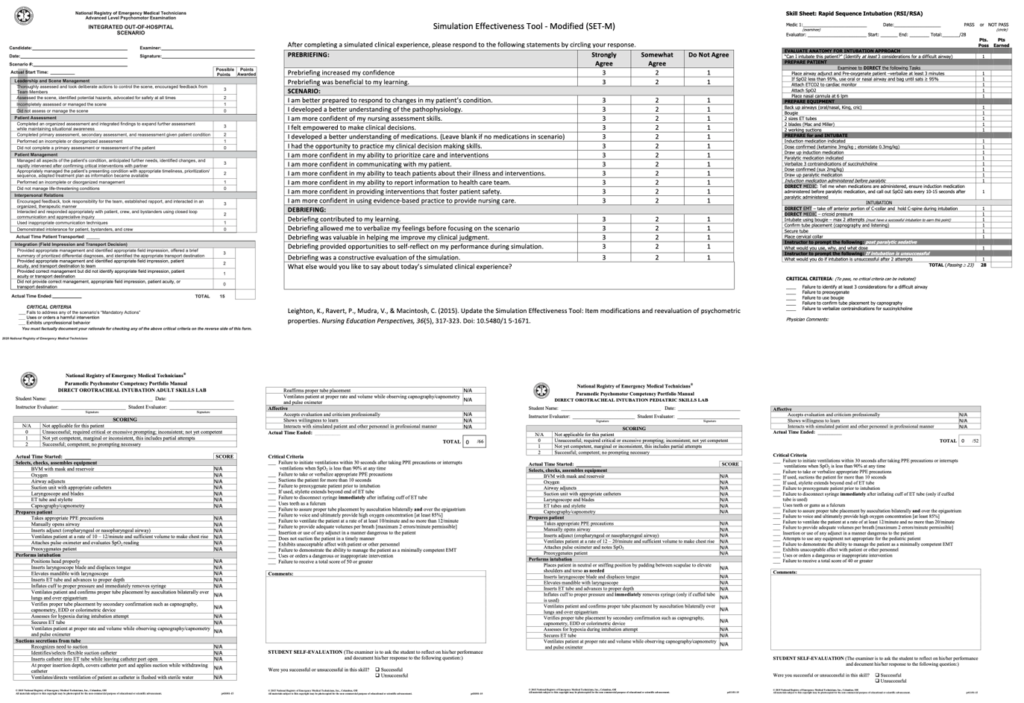
Criterion 10: Developing an evaluation plan.
Based on Kirkpatrick’s model, the four levels, reaction, learning, behavior, and outcomes, are useful strategies for evaluating different stages of SBT.14 Moreover, the evaluation process, including the assessment and feedback framework, is essential to determine the quality and effectiveness of the SBT experience. The evaluation forms, such as electronic Patient Care Report (PCR), were adopted and will be modified accordingly to evaluate the learning process and performance of the candidates.15-18
Criterion 11: Pilot test simulation-based experiences before full implementation.
The whole process of the SBT program for paramedics will be tested as a pilot study before the full implementation of the program.
8. Conclusion
The simulation-based training program should be designed according to the paramedics’ level with detailed instructions and consistent and effective feedback on their performance. This project was aimed to develop an ETI-SBT-On-the-Go program for continuing professional development to be accredited by the Saudi Commission for Health Specialties to enhance and maintain the endotracheal intubation skills for paramedics with infrequent intubation attempts in out-of-hospital settings. The proposed program will be personalized in design and depends on the assessment of paramedics’ level and their performance according to the data obtained from the electronic patient care reports of the Saudi Red Crescent Authority for each candidate. The program framework will be tested before SCFHS accreditation and full implementation.
9. References
- Bienstock, Jared, Albert Heuer, and Yingting Zhang. “Simulation-Based Training and Its Use Amongst Practicing Paramedics and Emergency Medical Technicians: An Evidence-Based Systematic Review.” International Journal of Paramedicine 1 (2023).
- Department of Health and Social Care (DHSC) website. Last retrieved May 06, 2023, from: https://committees.parliament.uk/writtenevidence/113067/pdf/.
- Henderson, Tristan, et al. “Examining the type and frequency of incidents attended by UK paramedics.” Journal of Paramedic Practice 11.9 (2019): 396-402.
- Dorsett, Maia, et al. “Prehospital airway management training and education: an NAEMSP Position Statement and Resource Document.” Prehospital Emergency Care 26.sup1 (2022): 3-13.
- Lyng, John, et al. “Prehospital pediatric respiratory distress and airway management training and education: an NAEMSP position statement and resource document.” Prehospital Emergency Care 26.sup1 (2022): 102-110.
- Annoni, Filippo, et al. “Brain protection after anoxic brain injury: Is lactate supplementation helpful?.” Cells10.7 (2021): 1714.
- Anderson, Jordan, Annalize Ebeid, and Catrin Stallwood-Hall. “Pre-hospital tracheal intubation in severe traumatic brain injury: a systematic review and meta-analysis.” British Journal of Anaesthesia (2022).
- Pilbery, Richard. “How do paramedics learn and maintain the skill of tracheal intubation? A rapid evidence review.” British Paramedic Journal 3.2 (2018): 8.
- Nørregaard, Annette, et al. “Safe transfer of simulation-based intubation skills to patients in cardiac arrest.” Journal of Paramedic Practice 10.3 (2018): 104-110.
- Lammers, Richard L., et al. “Comparison of four methods of paramedic continuing education in the management of pediatric emergencies.” Prehospital Emergency Care 26.4 (2022): 463-475.
- Lyng, John, et al. “Prehospital pediatric respiratory distress and airway management training and education: an NAEMSP position statement and resource document.” Prehospital Emergency Care 26.sup1 (2022): 102-110.
- Dorsett, Maia, et al. “Prehospital airway management training and education: an NAEMSP Position Statement and Resource Document.” Prehospital Emergency Care 26.sup1 (2022): 3-13.
- Watts, Penni I., et al. “Healthcare simulation standards of best practiceTM simulation design.” Clinical Simulation in Nursing 58 (2021): 14-21.
- Adamson, Katie Anne, Suzan Kardong-Edgren, and Janet Willhaus. “An updated review of published simulation evaluation instruments.” Clinical Simulation in Nursing 9.9 (2013): e393-e400.
- Simulation Effectiveness Tool -‐ Modified (SET-‐M) After completing a simulated clinical experience, please respond to the following statements by circling your response. Leighton, K., Ravert, P., Mudra, V., & Macintosh, C. (2015). https://www.caehealthcare.com/media/docs/Simulation-Effectiveness-Tool.pdf.
- National Registry of Emergency Medical Technicians (ADULT SKILLS LAB) Website. Last retrieved May 11, 2023, from: https://www.nremt.org/CMSPages/GetAmazonFile.aspx?path=~%5Cstorage%5Cmedia%5Cnational-registry%5Cnremt-documents%5Cfp410-direct-orotracheal-intubation-adult.pdf&hash=cd6222eb24d9955d904409ef1b1917a6cfdb3cd059b832464a5ad4da7bd86dd0.
- National Registry of Emergency Medical Technicians (PEDIATRIC SKILLS LAB) Website. Last retrieved May 11, 2023, from: https://www.nremt.org/CMSPages/GetAmazonFile.aspx?path=~%5Cstorage%5Cmedia%5Cnational-registry%5Cnremt-documents%5Cfp411-direct-orotracheal-intubation-pediatric-skill-lab-form.pdf&hash=bf88e2d0dd19c51f2774a1ebc6fb535e5d958919365037edaee2e0eae3846516.
- Skill Sheet: Rapid Sequence Intubation Website. Last retrieved May 11, 2023, from: https://www.regionsems.com/wp-content/uploads/2016/04/2013-RSI-SKILLS-SHEET_9-30-13.pdf.
- Freytag, Julia, et al. “Improving patient safety through better teamwork: how effective are different methods of simulation debriefing? Protocol for a pragmatic, prospective and randomized study.” BMJ open 7.6 (2017): e015977.
- Prakash, Shivesh, et al. “Prospective randomized controlled trial of video-versus recall-assisted reflection in simulation-based teaching on acquisition and retention of airway skills among trainees intubating critically ill patients.” Critical care medicine48.9) (2020): 1265-1270.
10. Appendices: Evaluation forms for the SBT Program.
Rawan Alghamdi, NRP, BSc EMS, is a paramedic working with the Saudi Red Crescent Authority (SRCA). She is a certified BLS instructor. She is completing her master’s degree in medical education at King Abdulaziz University in Saudi Arabia.
Ashraf Almahwasi, MSc, PhD, MIPEM, is a consultant and director of Medical Physics and Radiation Safety at the SFHM. He is a certified SCFHS TOT-facilitator, item author, surveyor and is an IAEA TTTRPOs trainer who provides training to postgraduate residents and radiation protection officers in several training centers. He is a board member and a designated institutional officer of the volunteer platform at the SMPS. He is a researcher in radiobiology and medical education.



