A crew arrives on scene at the rural home of a 22-month-old male in respiratory distress. The patient has weak peripheral pulses, and breath sounds reveal scattered rhonchi – with intercostal and suprasternal retractions – and nasal flaring. As a non-rebreather mask (NRBM) is placed on the child, the father states, “He’s been breathing like this for two days” (that’s right, two days!), and “he hasn’t been eating normally for three days.” The child is placed on the monitor and the vital signs observed are: heart rate 133, respiratory rate 57, blood pressure 92/55, O2 saturation 88% on room air and temperature 38.3C. The NRBM flow is set at 12 LPM but the patient continues breathing at a rate of 55 breaths-per-minute with no improvement in the retractions or nasal flaring.
Oxygen consumption during transport must be carefully considered. You have 1,200 PSI in your on-board M tank, and the closest hospital is 95 minutes away. If oxygen delivery is calculated (See previous article, “What? We Ran Out of Oxygen?”), the current liter flow of 12 LPM will allow only 91 minutes for transport time. An alternative plan must be selected.
One option would be to decrease the flow of oxygen delivered, as a child this size might not require a 12 LPM flow. Assuring a tight seal with the mask, reduce the flow of oxygen while observing the reservoir bag, verifying that the bag does not deplete as the patient inhales. Ideally, the reservoir bag should remain at least 1/3 to 1/2 full in between respirations. Dropping the flow to 8 LPM allows 136 minutes of oxygen available for the patient.
An alternative would be to select a more specific oxygen delivery device for the patient’s current condition. A NRB mask can deliver approximately 60-90% FiO2 but does nothing to address the tachypnea, retractions and nasal flaring issues. These are clear indications of an increase in airway resistance, resulting in an increased work of breathing. Placing a NRB mask on this patient does little to reduce the work of breathing.
Some modalities used in hospitals may be beneficial in the transport arena. Typically, these children receive some form of oxygen delivery to start, but may need chest physiotherapy (CPT) along with deep suctioning to mobilize secretions that add to airway resistance.
If no improvement is noted, the next modality to be considered is high flow nasal cannula (HFNC). The severity of symptoms guides the amount of flow per kg, with maximum flow targeted at 2L/kg. The severity level is determined by respiratory rate, retractions and breath sounds. If patient condition warrants escalation, CPAP or BiPap might be the next modality of choice. This can be tricky with children as sizing of masks and patient compliance can be difficult mission.
An exploration of underlying causes for this common scenario might reveal respiratory syncytial virus (RSV). RSV was first described as acute catarrhal bronchitis in 1901.1 This virus causes acute respiratory tract illness in persons of all ages. In fact, almost all children are infected by two years of age, and reinfection is common.2 RSV symptoms are usually mild and will often resemble a common cold in adults and healthy children. However, the infection may migrate to the lower respiratory tract, resulting in pneumonia or bronchiolitis. These conditions will eventually affect airway resistance and lung compliance. Signs and symptoms include: tachypnea, hypoxia, cyanosis, fever, severe cough, wheezing, retractions and poor feeding.
The typical “season” for RSV in the United States is from late fall to early spring, with a spike in late January into February. However, social distancing for COVID-19 during the winter of 2021 resulted in a lower than usual rates of RSV, followed by an unusual spike cases through the succeeding summer months. Some experts believe this is due to the relaxing of social distancing and parents’ return to work, requiring infants and young children to return to the congregate environments of daycare, pre-schools and social activities.3
Current treatment for mild cases of RSV is simply supportive care. The main goal is to maintain hydration and nutrition along with oxygen saturations greater than 90%. Evidence-based clinical recommendations suggests that bronchodilators, systemic or inhaled corticosteroids, and epinephrine should not be administered to infants and children with bronchiolitis.4
As previously discussed, the NRB mask is the “go to“ modality for very low oxygen saturations, improving numbers on your monitor, but doing nothing about the increased work of breathing. High-flow nasal cannulas designed specifically for transport may be a good alternative to alleviate the airway resistance caused by increased secretions. Most dedicated neonatal/pediatric transport teams will have access to HFNC’s in their transport units. It is important to note that the delivery of high flows should be heated and humidified, and include a blender for precise FiO2 delivery.
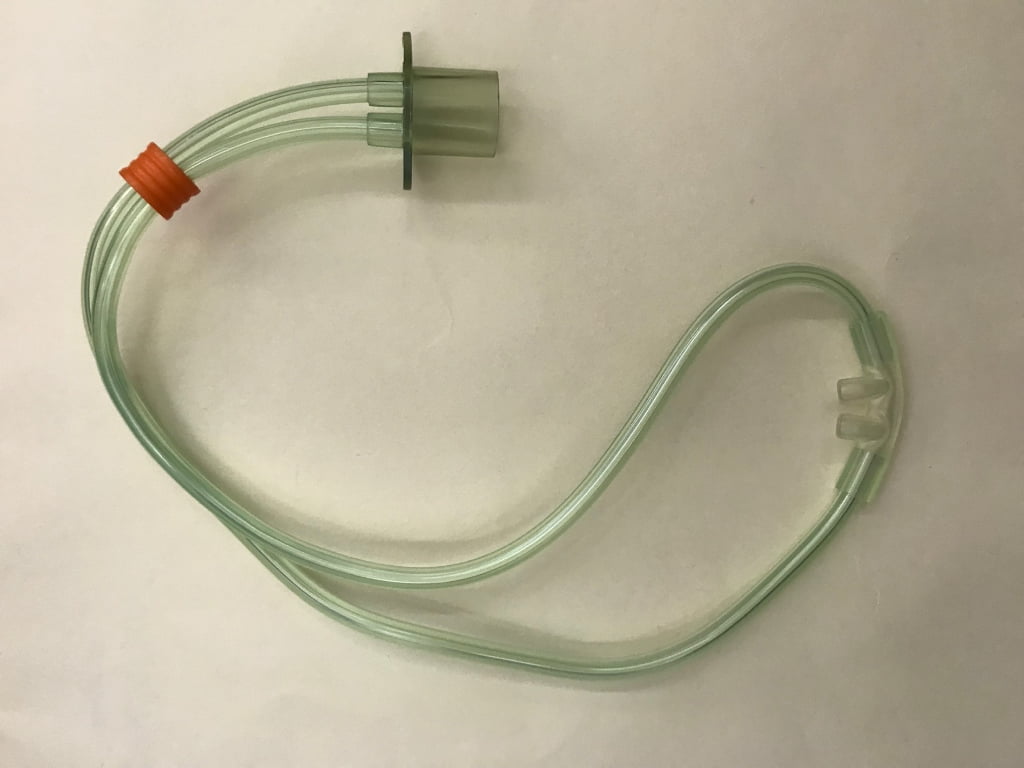
Ram Cannula (Photo courtesy of Jeremy Fails, Air Med)
Another device currently in use for transports is the RAM cannula, which can be used as a low or high flow nasal cannula. One of the great advantages to this device is it can also be connected to a ventilator circuit which allows the application of CPAP or BiPap if needed. This therapy should only be utilized by respiratory therapists, nurses or paramedics specially trained for critical care transport.
There is more awareness of the need for transporting patients on high-flow nasal cannula since the COVID-19 pandemic. The Hamilton T-1 transport ventilator is now being equipped with HFNC software to provide flows up to 60/LPM.
As with any transport, accurate assessment, vigilant monitoring and appropriate treatment is essential. For the pediatric population, it is imperative to continually assess the level of respiratory distress, watching for subtle changes, as there is a fine line between respiratory distress and respiratory failure in this high-risk population. A small percentage of these patients may even require intubation and mechanical ventilation. Infants and children do not have the reserve of adults and can deteriorate quickly. Additionally, they cannot communicate their level of distress. This is where training and assessment skills can shine, transporting patients in safety and comfort.
References
- Principles and Practice of Pediatric Infectious Diseases, 2nd New York, NY Churchill Livingston; 2003:213—218
- Committee on Infectious Diseases. American Academy of Pediatrics. 2009; 124:1694
- Ujiie, M., Tsuzuki, S., Nakamoto, T., Iwamoto, N. Resurgence of respiratory syncytial virus infection during COVID-19 pandemic, Tokyo, Japan. Emerg Infect Dis. 2021 Nov (September 27, 2021) https://doi.org/10.3201/eid2711.211565
- Ralston SL, Lieberthal AS, Meissner HC, et al.; American Academy of Pediatrics. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis [published correction appears in Pediatrics. 2015;136(4):782]. Pediatrics. 2014;134(5):e1474–e1502
Michael Schauf, RRT-NPS, has been a registered respiratory therapist at Albany Medical Center Hospital in New York since 1994. He covers all in-patient units, ICUs, the adult and pediatric Emergency Departments and is a member of the neonatal/pediatric transport team at this Level I Trauma and Level 3 NICU Center. Michael is the founder of Vent-Pro Training, teaching medics and nurses around the world how to manage mechanically ventilated patients during ground, rotor, and fixed-wing transports. He has been a flight respiratory therapist since 1998, currently working for AirMed and as a clinical education specialist for AMR. Michael authored the respiratory chapter of, “Critical Care Transport, 2nd edition,” published by Jones & Bartlett and is an adjunct instructor in the Respiratory Care Program at Hudson Valley Community College.


