
Photo provided by the author.
By John Wheeler, BHS, LP, FP-C
The High Stakes of Prehospital Intubation
Rapid sequence intubation (RSI) is widely recognized as one of the most technically demanding and high-risk procedures performed by paramedics in the prehospital setting. The stakes are immense – a failed airway can rapidly lead to hypoxia, aspiration, or cardiac arrest.
Despite the gravity of RSI, many EMS systems persist in using standard geometry blades – tools that require complex head positioning, forceful lifting, and precise axis alignment to visualize the glottis effectively. These outdated blades not only complicate intubation but also increase the risk of failed attempts, particularly in anatomically challenging airways.1
In contrast, hyperangulated can improve first pass success rates, reduce cognitive load, have proven superiority in difficult airways, and improve patient outcomes.
Hyperangulated laryngoscopes provide a more anatomically adaptive approach, allowing for superior glottic exposure without excessive manipulation. Data from PCHD EMS in 2023 underscores the impact of this approach, demonstrating a 96.88% first-pass success rate using hyperangulated blades with a specifically designed rigid stylet exclusively.2
This consistency highlights the critical advantage of simplifying laryngoscope choices, allowing paramedics to refine their technique and improve outcomes. The practice of medicine demands that we not only provide our patients with date driven care, but that we also make sure that our skills align with that care. At Parker County (TX) Hospital District EMS, we have found that keeping things simple has the most profound effect.
In emergency airway management, where seconds count and second chances are rare, hyperangulated blades are not just a recommendation – they are a necessity. While the benefits of hyperangulated video laryngoscope are clear, it’s essential to note that any provider performing rapid sequence intubation must practice regularly to maintain proficiency.
Standard Geometry vs. Hyperangulated
On the other hand, standard geometry laryngoscopes, such as the Macintosh blade, require alignment of the oral, pharyngeal, and tracheal axes to visualize the glottis directly. This technique often demands significant head extension and upward lifting – maneuvers that can be particularly challenging in patients with cervical spine injuries or confined spaces.
Conversely, hyperangulated video laryngoscopes (HAVLs) feature a sharply curved blade, allowing for indirect visualization via a camera, bypassing the need for axis alignment.3 This design is particularly advantageous in anatomically difficult airways, minimizing the need for excessive head manipulation.
Often times, EMS agency supply providers with a wide variety of options to address a given problem. While this approach has numerous benefits, in high acuity situations, keeping an approach simple has its own benefits.
The Dunning-Kruger Effect
The Dunning-Kruger effect – the cognitive bias where individuals with limited competence overestimate their abilities – is particularly relevant in EMS airway management.
Paramedics, equipped with various laryngoscopes but limited intubation opportunities, may falsely perceive themselves as proficient after a few successful placements. However, evidence suggests that true airway mastery requires repeated practice – a level of exposure few paramedics achieve in the field.
By offering multiple laryngoscope options without emphasizing consistent, repetitive training with a single device, EMS systems may inadvertently foster false confidence, increasing the risk of failed intubations.4
Life or Death in Seconds
Imagine a critical airway scenario: A paramedic is kneeling over a rapidly deteriorating patient, the airway obstructed, time running out. The paramedic reaches for a laryngoscope – but which one?
Hyperangulated or standard geometry? In these moments, the wrong choice can mean the difference between life and death. Despite mounting evidence that hyperangulated blades enhance visualization in difficult airway scenarios, many EMS systems continue to offer multiple laryngoscope options, potentially diluting expertise and delaying mastery.5
The argument here is clear: airway management success is not about more tools – it’s about fewer, better tools. Standardizing hyperangulated laryngoscopy could simplify training, reduce cognitive load, and ultimately save lives.
Overcoming Resistance to Change
Resistance to change is a deeply rooted issue in EMS, shaped by a culture that values tradition and repetition. Emergency medical protocols become ingrained through years of training, creating a sense of security in familiar methods. Introducing new techniques or equipment disrupts that comfort zone, potentially threatening a provider’s perceived competence.6
Many paramedics have seen “innovative” protocols come and go without delivering on their promises, leading to skepticism toward new practices. The Dunning-Kruger effect further complicates this issue; less experienced providers may cling to outdated techniques they feel comfortable with, dismissing newer approaches as unnecessary. This entrenched adherence to “what has always worked” can impede progress and perpetuate suboptimal methods, potentially compromising patient outcomes.
Real-World Results
PCHD EMS, consisting of approximately 90 paramedics, had a 70% first-pass success rate with standard geometry laryngoscopes before transitioning to hyperangulated blades. The 2023 data from PCHD EMS underscores the effectiveness of hyperangulated laryngoscopy, showing a 96.88% first-pass success rate using the GlideScope Go with a rigid stylet for RSI procedures.
This result notably exceeds national averages for prehospital intubation, typically ranging between 77-85%.1 Despite occasional fluctuations, such as October (85.17%) and December (92%), the overall trend suggests that standardizing hyperangulated blades can mitigate variability in paramedic performance. EMS agencies that limit laryngoscope options and emphasize consistent, targeted practice are likely to see improved skill retention and better patient outcomes.
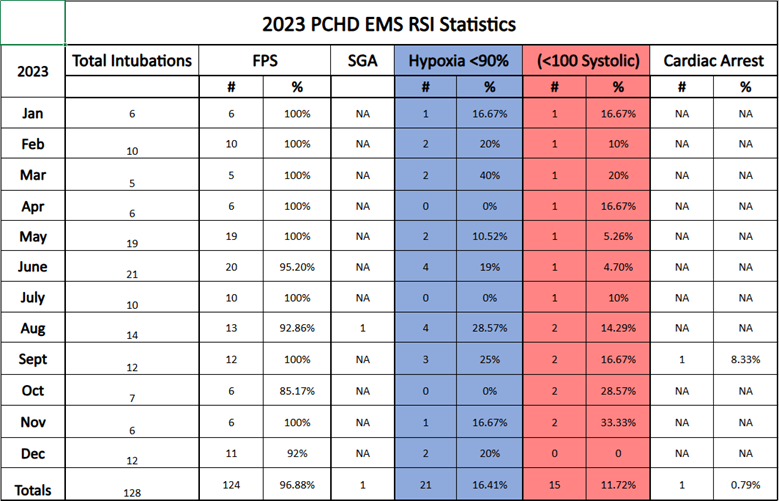
Data provided by Parker County Hospital District.
Considerations for Pediatric Patients
While our data and clinical experience at PCHD EMS are limited to adult patients, the broader argument for hyperangulated video laryngoscope remains compelling. Pediatric airway management presents unique challenges, such as smaller anatomy and a long, floppy epiglottis, which have traditionally favored straight blades like the Miller.
Conclusion
With proper training and consideration of patient anatomy, hyperangulated approaches may also offer advantages in select pediatric cases. Still, further real-world clinical research is needed to confirm these benefits across younger populations.
About the Author
John Wheeler, BHS, LP, FP-C, is a field supervisor and critical care paramedic with Parker County Hospital District EMS in Texas. He has over 13 years of experience in prehospital care and holds a Bachelor of Science in Health Sciences. He is dedicated to advancing EMS education and improving clinical outcomes through high-performance training and protocol innovation.
References
1. Wang, H. E., Seitz, S. R., Hostler, D., Yealy, D. M., & Lave, J. R. (2021). Association Between Emergency Medical Service Agency Intubation Success Rates and Patient Outcomes. Annals of Emergency Medicine, 78(2), 165–174. https://doi.org/10.1016/j.annemergmed.2021.01.008
2. PCHD EMS. (2023). Internal performance data on first-pass success rates using GlideScope Go.
3. Downey, A. W., Duggan, L. V., & Law, J. A. (2023). Video laryngoscopy versus direct laryngoscopy for out-of-hospital orotracheal intubation: A systematic review and meta-analysis. PubMed. https://pubmed.ncbi.nlm.nih.gov/37256300/
4. Yang, W.-S., Yen, P., Wang, Y.-C., Chien, Y.-C., & Chiang, W.-C. (2022). Objective performance of emergency medical technicians in the use of mechanical cardiopulmonary resuscitation compared with subjective self-evaluation: A cross-sectional, simulation-based study. BMJ Open, 12(6), e062908. https://doi.org/10.1136/bmjopen-2022-062908
5. Air Medical Journal. (2021). A randomized controlled crossover trial. Air Medical Journal, 40(3), 123-129. https://doi.org/10.1016/j.annemergmed.2021.01.008
6. Nieman, J. (2023). Resistance to change in the emergency services. LinkedIn. https://www.linkedin.com/pulse/resistance-change-emergency-services-jo-nieman-ahoye
Exclusive feature content from thought leaders in airway management.


