
John Wheeler
By John Wheeler
Abstract
Advanced airway management remains one of the most scrutinized and misunderstood aspects of prehospital care. Despite its proven benefits, a persistent myth suggests that patients who receive intubation in the field often die shortly afterward.
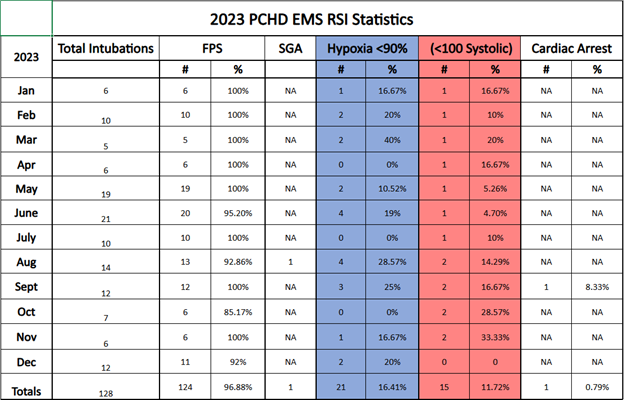
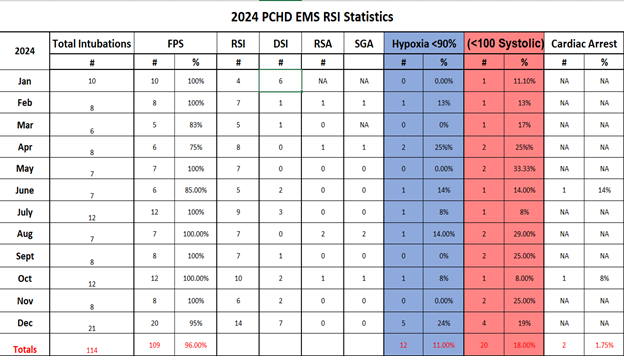
This retrospective analysis of 242 advanced airway cases from Parker County (TX) Hospital District (PCHD) EMS, in Weatherford, Texas, between 2023 and 2024 reveals consistently high first-pass success (FPS) rates and low complication frequencies.
The data directly challenges the perception that advanced airway management is inherently harmful. Instead, they reinforce that skilled EMS providers, following structured protocols and education, can achieve safe and effective airway outcomes.
At PCHD, all paramedics complete a dedicated advanced airway management course led by critical care instructors, including the following:
- Didactic education.
- Simulation.
- A written examination.
- Scenario-based competency assessments.
Each paramedic is also recredentialed annually to ensure continued competency and adherence to evolving best practices. Our findings support the growing body of literature advocating for evidence-based airway practices and training in the prehospital setting.
Introduction
Among EMS providers, one of the most dangerous myths is the belief that patients “just die” after advanced airway management. It is often rationalized with statements like, “Well, they were really sick anyway,” or “They probably would have died no matter what.”
While these sentiments may offer emotional insulation for clinicians, they oversimplify the complexity of critical care and ignore the impact of skillfully executed airway management. This mindset can lead to therapeutic inertia, hesitation, and missed opportunities to improve outcomes.
The truth is that when it’s done right, advanced airway management, including resuscitation sequence intubation (RSI), delayed sequence intubation (DSI), and rapid sequence airway (RSA), saves lives. This paper reviews 2023 and 2024 airway management data from PCHD EMS, which has used hyperangulated video laryngoscopy and a standardized RSI protocol for nearly a decade.
The objective is to examine airway outcomes, quantify complication rates, and highlight how clinical proficiency and protocol adherence lead to safer, more effective airway management in the field.
Methods
A retrospective review was conducted on all RSI cases performed by PCHD EMS in 2023 and 2024. Data were extracted from the agency’s internal airway registry and quality assurance records.
Cases were analyzed based on total intubations, first-pass success, hypoxia (<90% SpO2), hypotension (<100 mmHg systolic), supraglottic airway (SGA) use, and cardiac arrest following airway intervention. Hypoxia and hypotension were evaluated using the DASH-1A standard, which assesses physiologic stability within 10 minutes post-intubation.1
This methodology focuses on post-intubation values to benchmark the safety and effectiveness of advanced airway procedures, and is a widely accepted metric in prehospital airway performance evaluation.
Results
Across the two-year period, a total of 242 advanced airway attempts were documented.
- FPS: Out of 242 total intubations, 233 were successful on the first attempt, representing a combined FPS rate of 3%.
- Hypoxia Events: Hypoxia occurred in 33 of 242 cases, a combined rate of 6%.
- Hypotension Events: Post-intubation hypotension (<100 systolic) occurred in 35 of 242 cases (5%).
- Cardiac Arrest Following Intubation: Only 3 patients (1.2%) experienced cardiac arrest post-airway management.
- SGA Utilization for RSA: SGA devices were used in just 1 case in 2023 and 8 cases in 2024, demonstrating the agency’s strong reliance on definitive airways when clinically appropriate.
Notably, 2024 saw expanded use of DSI (15 cases) and RSA (3 cases), reflecting the agency’s adoption of modern airway strategies to optimize oxygenation and hemodynamics.
Discussion
The results from Parker County EMS clearly refute the notion that patients die as a direct result of field intubation. With a 96.3% first-pass success rate and minimal adverse events, the data align with national benchmarks and best practices outlined in airway management literature.
Recent studies have demonstrated that prehospital advanced airway management, when performed by trained providers using appropriate equipment and preoxygenation strategies, improves outcomes in critically ill patients.2,3
Complication rates such as hypoxia and hypotension are typically associated with delayed or multiple attempts, not the procedure itself.4
PCHD EMS has implemented key interventions shown to reduce airway complications:
- Mandatory GlideScope Go VL with hyperangulated blades.
- Standardized RSI checklists.
- Focused training on preoxygenation and resuscitation before induction.
- Ongoing QA reviews of every RSI.
These data-driven practices improve both technical performance and clinical judgment. Furthermore, the use of DSI and RSA represents an evolving understanding of airway physiology, favoring preparation over haste.
We must begin holding ourselves accountable to the data, not the folklore. When patients deteriorate post-intubation, we should ask whether the intervention was timely, appropriately executed, and adequately supported with preoxygenation and resuscitation—not simply default to the idea that they were going to die anyway.
Conclusion
The belief that patients routinely die after advanced airway management is unfounded. The two-year performance of PCHD EMS demonstrates that with proper training and equipment as well as clinical judgment, airway management is a lifesaving intervention.
The narrative must shift away from fear and toward evidence. Paramedics are not causing harm with intubation. When skilled EMS providers operating under structured protocols and supported by focused education perform intubation, they are saving lives.
About the Author
John Wheeler is a critical care field supervisor at Parker County (TX) Hospital District EMS. With 13 years of paramedic experience, he specializes in advanced airway management. Wheeler has a bachelor’s degree in health science and the FP-C certification. He serves as a lead airway instructor, training paramedics in advanced airway techniques in prehospital care.
References
1. Miller, L. R., Spelten, O., Lawton, B., Mechem, C. C., & Wang, H. E. (2020). DASH-1A: A performance measure for evaluating advanced airway management in out-of-hospital cardiac arrest. Prehospital Emergency Care, 24(5), 647–654.
2. Wang, H. E., Schmicker, R. H., Daya, M. R., et al. (2018). Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest. JAMA, 320(8), 769-778.
3. Jarvis, J. L., Gonzales, M., Johns, D., & Brown, L. H. (2021). Implementation of a performance improvement program for prehospital airway management. Prehospital Emergency Care, 25(1), 27-35.
4. Heffner, A. C., Swords, D. S., Neale, M. N., & Jones, A. E. (2020). Incidence and factors associated with cardiac arrest complicating emergency airway management. Annals of Emergency Medicine, 75(1), 16-22.
Exclusive feature content from thought leaders in airway management.



thank you for your contribution to the airway literature. Just curious, do you use paralytics?
I really appreciate the kind words. Yes, we use Rocuronium as our neuromuscular blocking agent. It’s the only paralytic we carry.
I really enjoyed reading this. Is there any way you could possibly share your training for airway? I am currently trying to build a program up and make the numbers better. Thank you.
Sorry for the late reply. Thank you so much, and I really appreciate the kind comment. We have a very structured airway course that covers the 7P’s of RSI/DSI/RSA. The education is very in-depth and includes scenario-based training and hands-on skills. We cover preoxygenation strategies, resuscitation-focused, and human factors. Hope this helps.