Introduction
In the United States, respiratory complaints account for approximately 10 million emergency department visits per year, representing about 10% of all chief complaints.1 Prehospital providers are frequently called to assess and treat respiratory distress, which can arise from both acute and chronic conditions. Out-of-hospital treatment of these conditions has been shown to reduce mortality and improve patient outcomes.2
The assessment and treatment of respiratory and pulmonary pathologies requires a thorough history, physical exam, clinical assessment and prompt initiation of treatment to prevent patient decompensation or death. Differentiating between pulmonary diseases is key in providing the correct and adequate treatment. Many of these diseases share similar words and phrases, leaving little room for error in communicating with patients, providers, and receiving facilities. This article seeks to help define some of the more common pulmonary pathologies and help prehospital providers differentiate between these causes of respiratory distress.
Pulmonary Anatomy and Physiology
To set the stage for the discussion, we will start with an overview of pulmonary anatomy and physiology. The purpose of the lungs is to provide an interface for gas exchange from the blood, bringing oxygen into the body and carbon dioxide out of the body.
This requires:
- Blood to be brought into and then out of the lung tissue (perfusion),
- Air to be brought into and out of the airways (ventilation),
- A place for the exchange to occur.
The lung itself also must be able to expand and contract in order to provide the pressure changes necessary to complete these cycles of exchange.
For the purposes of this review, we will trace the pathway of blood returning to the heart from the venous system (deoxygenated, carbon dioxide rich), through the lungs, and then back out into arterial circulation (oxygenated, carbon dioxide poor).
Figure 1 provides a diagram of this process and its components. First, venous blood is drained into the right atrium through the superior and inferior vena cava. From the right atrium, blood is pushed into the right ventricle, then out into the pulmonary artery. The pulmonary artery splits into a right and left component and continues to branch out until it becomes a capillary at the alveoli of the lung.
The alveoli represent the terminal units of the airway, coming from trachea to bronchus to bronchiole and then at the end of each bronchiole are several groups of alveoli. Capillaries form a net-like structure around these alveoli and typically have a single-layer cell wall to facilitate gas exchange. At the capillary-alveolar interface, through a series of chemical reactions and diffusion principles beyond the scope of this article, oxygen is brought into the blood and attaches to hemoglobin, while carbon dioxide diffuses out of the blood and into the lungs for expiration.
Once the exchange occurs, the carbon dioxide is expired and the oxygenated blood returns to the heart via the pulmonary vein, where it flows into the left atrium, followed by the left ventricle, and then aorta which propels oxygenated blood into systemic arterial circulation. While these exchanges are occurring, the lung physically expands and contracts within the chest, sliding against the chest wall and pleura, a layer of protection around the lung that allows for lubrication and cushioning for lung expansion and contraction.
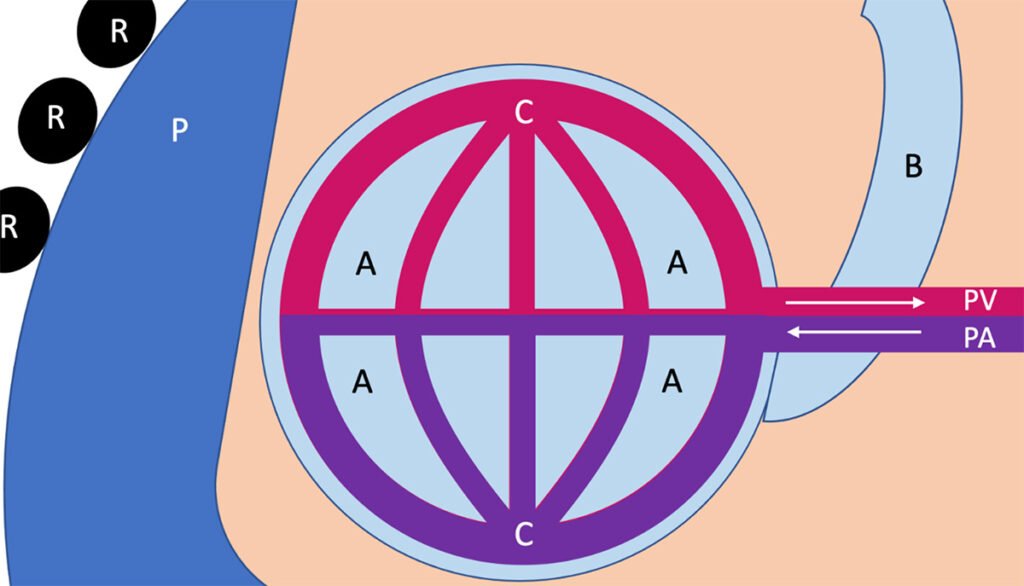
Figure 1: A Basic Overview of Pulmonary Anatomy and Physiology [A = Alveoli, B = Bronchiole, C = Capillary, PA = Pulmonary Artery, PV = Pulmonary Vein, P = Pleura, R = Rib]
The Ps and Es of Pulmonary Pathology
This review is not meant to be all encompassing. Rather, it focuses on four commonly confused pulmonary disease processes. Each can be an acute process or related to an underlying chronic condition. Envision these processes in one of three spaces: the blood vessels (pulmonary artery/vein, capillaries), the airway (bronchioles and alveoli) or pleura (outside the lung, between the chest wall and the lung tissue).
1. Pulmonary Embolism
In a pulmonary embolism, a clot in the pulmonary arterial system prevents perfusion of the capillaries surrounding the alveoli (Figure 2). This prevents gas exchange from taking place and leads to profound hypoxia. These patients may present with acute onset shortness of breath, hypoxia not responsive to oxygen therapy, tachycardia, and extreme dyspnea. Patients may or may not complain of chest pain or tightness. Hemoptysis (coughing up blood) is a relatively uncommon symptom but can also be present.
Lung auscultation may reveal normal or slightly diminished breath sounds, especially at the bases. Pulmonary embolism has a unique set of risk factors including recent surgery, immobilization, atrial fibrillation, hypercoagulable disorders, history of cancer or cancer treatment, and a history of other clots, such as a deep venous thrombosis (DVT). Treatment of pulmonary embolism in the pre-hospital setting includes supportive care such as high-volume oxygen administration, EKG monitoring, and establishing IV access.
Pharmacologic agents used in the treatment of pulmonary embolism include thrombolytics, such as tissue plasminogen activator (TPA) or intravenous heparin administration. These should be administered in consultation with on-line medical command and per local protocols.
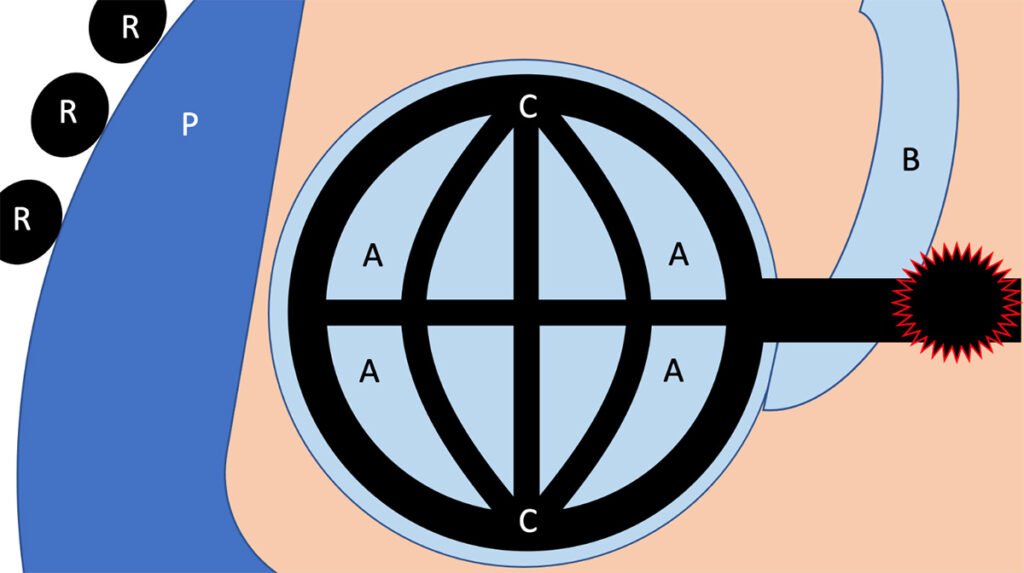
Figure 2: Pathologic Process of a Pulmonary Embolism. [Embolism outlined in red].
2. Pulmonary Edema
When pulmonary edema occurs, fluid from the vascular space crosses the capillary into the alveoli, typically as a result of high pressures within the capillary from volume overload or heart failure (Figure 3). In volume overload, the amount of fluid within the capillaries is too much and the excess is pushed into the alveoli. In heart failure, backpressure from the left atria and ventricle leads to fluid being pushed across the capillary membrane and into the alveoli. In both cases, this excess fluid prevents gas from being exchanged across the capillary. These patients present with dyspnea, productive cough, and jugular venous distension.
They may have symmetric edema elsewhere in their body, such as the lower extremities. Vital signs will show tachycardia, hypoxia that is usually responsive to supplemental oxygen therapy, and hypertension. Patients with pulmonary edema will often experience positional changes in their symptoms, with worsening shortness of breath while lying down.3 It is important to allow these patients to sit up or position themselves in such a way that their symptoms improve. Lung sounds will reveal rhonchi or wheezing that is worse at the bases of the lungs, especially in a Fowler or semi-Fowler position.
Often these patients have a component of chronic cough and shortness of breath, as there are a number of chronic conditions that can lead to pulmonary edema. These include renal failure and patients on dialysis, left or right heart failure, pancreatitis, or liver failure. For patients with these chronic conditions, it is important to inquire about medication history and compliance, recent weight changes, disease history, and symptom evolution.
Treatment for these processes focuses on two goals: reducing the amount of fluid in the alveoli and reducing the amount of fluid in the body overall. Continuous positive airway pressure (CPAP) may be helpful in physically pushing the fluid back across the capillary membrane and into systemic circulation. Diuretics, such as furosemide or bumetanide, may also be used to decrease the amount of fluid in circulation through renal excretion. Care should be taken to minimize fluids given to these patients to prevent worsening of underlying fluid overload. In some cases, vasodilators, such as nitroglycerin, may also be used, but these should only be used if local protocols allow and in consultation with on-line medical command.
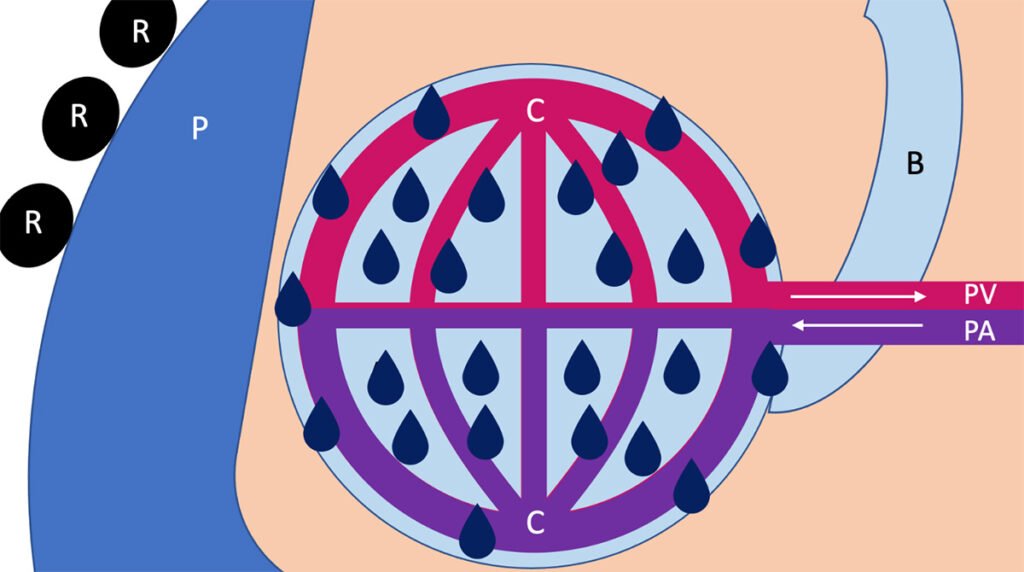
Figure 3: Pathologic Process of Pulmonary Edema
3. Pleural Effusion
When a pleural effusion occurs, fluid collects between the chest wall and the lung, in between layers of pleura (Figure 4). Normally, a thin layer of fluid (about 10-20 mL) separates the visceral (against the lung) and parietal (against the chest wall) layers of the pleura. In a pleural effusion, the amount of fluid between these two layers increases and compresses the underlying lung tissue. The pleural cavity can expand to accommodate as much as two liters of effusion, compressing the underlying lung tissue and preventing both ventilation and perfusion.
Pleural effusions can be unilateral or bilateral depending on their etiology. Infection of underlying lung tissue, such as in pneumonia, can lead to a unilateral pleural effusion. Volume overload, often as a result of the same chronic conditions that lead to pulmonary edema, can also lead to bilateral pleural effusions. Patients may complain of pleuritic chest pain (pain worsening with inspiration), shortness of breath, dyspnea, fevers, and cough. Dyspnea and shortness of breath will worsen as the effusions increase in volume, especially if the effusions are bilateral. Physical examination will reveal diminished breath sounds over the area of effusion, crackles, and potentially a “pleural rub” (crackles that worsen with expiration).
Treatment of pleural effusion relies on treating the underlying causes. If the cause is volume overload or increased vascular pressure, treatments are similar to those of pulmonary edema: ventilatory support with CPAP or supplemental oxygen with diuresis. As with pulmonary edema, care should be taken to minimize fluids given to these patients to prevent worsening of underlying fluid overload.
If there is an underlying inflammatory or infectious cause, such as pneumonia or pleural infection, management relies on treatment of the underlying process with antibiotics or anti-inflammatories, in addition to supportive measures. For large volume pleural effusions, surgical drainage may be required. Drainage of pleural effusions often necessitates additional laboratory analysis of the fluid composition to characterize the exact etiology of the effusion.
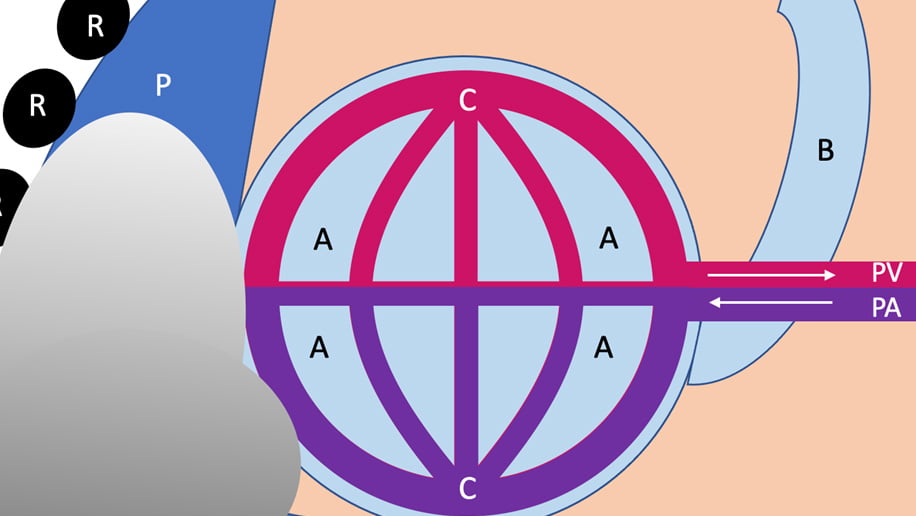
Figure 4: Pathologic Process of a Pleural Effusion
4. Pneumothorax (Pneumothoraces)
Pneumothoax (or pneumothoraces if bilateral) occurs when there is entry of air into the pleural space betweent the lung and chest wall. This results in physical compression of the underlying lung tissue, preventing lung expansion, impairing both ventilation and perfusion. The etiology of pneumothorax is most commonly from chest trauma, either internal disruption of the alveoli and visceral pleura, or externally from an open chest wound.
Air entry into the pleural space allows pressure to build, as air is sucked into the thoracic cavity with each inspiration, but not removed during expiration. As pressure builds, the lung can sequentially collapse until it is rendered nonfunctional. For large defects in the chest wall or underlying lung, the pneumothorax can exert enough pressure to shift the contents of the mediastinum (vena cava, heart, aorta, and trachea) away from the affected side.
Mediastinal shift causes characteristic tracheal deviation and impairs venous return to the heart, creating a tension pneumothorax. Without prompt intervention, patient decompensation is often imminent at this stage.
Outside of trauamtic etiologies, spontaneous pneumothoraces can occur in patients with underlying lung disease that weakens lung tissue, such as chronic obstructive pulmonary disease (COPD) or connective-tissue disorder such as Elhers-Danlos Syndrome. These patients may have a history of previous spontaneous pneumothorax or recent decline in lung function.
Patients with a pneumothorax will present with shortness of breath and pleuritic chest pain that acutely worsens with inspiration. Physical exam in these patients will reveal tachycardia, hypoxia that is typically responsive to oxygen therapy, and diminished breath sounds on the affected side. Signs of tension physiology include hypotension, tachycardia, tracheal deviation away from the affected side, jugular venous distension, and altered mental status.
For pneumothoraces without tension physiology, treatment involves supportive care with supplemental oxygen therapy, IV access, and management of any external wounds with an occlusive dressing (allows air out during expiration, but not in during inspiration). Avoid positive pressure ventilation in these patients as it can worsen the underlying air leak. For patients with large pneumothoraces and signs of tension physiology, rapid evacuation of the pneumothorax is advised through needle decompression.
Depending on local protocols, needle decompression is performed in the second intercostal space at the midclavicular line with a 14 gauge angiocath. If placed correctly and with the right indication, a rush of air is likely to be encountered following catheter placement. Careful patient monitoring before, during, and after needle decompression is paramount to ensure successful treatment.
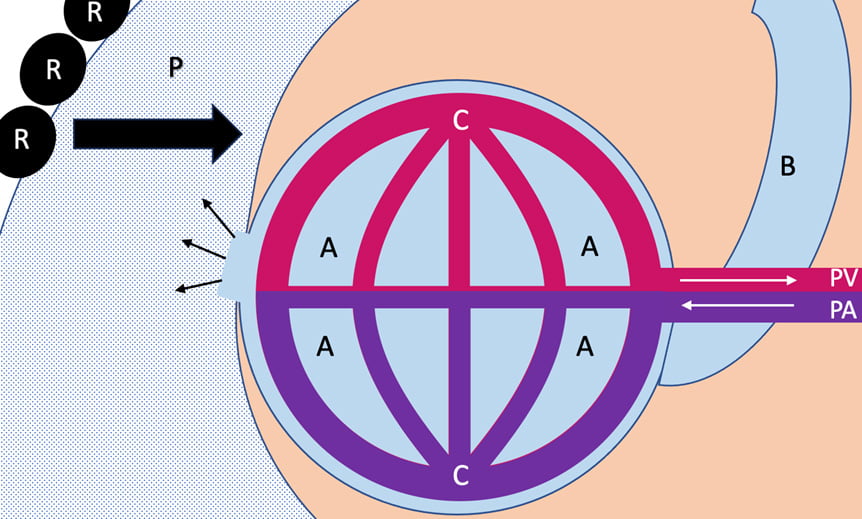
Figure 5: Pathologic Process of a Pneumothorax
Conclusion
Respiratory complaints remain one of the most common reasons for prehospital patient encounters. Differentiating between pulmonary diseases is key in providing the adequate and correct treatment. Pulmonary embolism, pulmonary edema, pleural effusion, and pneumothoraces all create respiratory distress, but have different underlying causes and distinct treatments.
By thinking through the anatomic spaces where pathology is occurring, the pathophysiologic processes, and the indicated treatments, prehospital providers can be better prepared to assess and treat patients. Finally, clear and timely communication of patient assessment with prompt transport to the receiving facility can help improve outcomes for patient with respiratory disease.
Key Words
Alveoli – the end (terminal unit) of the airway, this small air sac is surrounded by a network of capillaries to allow for gas exchange
Capillary – thin blood vessel that allows for diffusion of gas across the cell wall
Edema – an excess of fluid within the interstitial space, outside of cells and blood vessels
Effusion – an excess of fluid within a body cavity
Embolism – a blood clot that travels from elsewhere in the body and lodges within a vessel, halting blood flow past the point of obstruction
Pleura – the space between the lung and chest wall, consists of two layers: visceral, against the lung, and parietal, against the chest wall. An average of 10-20mL of fluid provides cushion and lubrication between these two layers
Pleural effusion – a collection of fluid outside of the lung tissue in the pleural space, can cause compression of the lung and inhibit ventilation and perfusion
Pneumothorax – a collection of air outside of the lung tissue in the pleural space, can cause compression of the lung and inhibit ventilation and perfusion
Pulmonary artery – blood vessel that carries oxygen-poor blood away from the heart to the pulmonary capillaries for gas exchange
Pulmonary edema – excess fluid collects within the alveoli, preventing the diffusion of gas across the
Pulmonary embolism – a clot in the pulmonary artery prevents blood from reaching the lungs and capillaries, preventing gas exchange and inducing hypoxia
Pulmonary vein – blood vessel that carries oxygen-enriched blood towards the heart and away from the pulmonary capillaries
References
1. Centers for Disease Control and Prevention. [Accessed Oct 15, 2023];National Hospital Ambulatory Medical Care Survey (NHAMCS) – 2021 emergency department summary tables. Available at: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2021-nhamcs-ed-web-tables-508.pdf
2. Stiell IG, Spaite DW, Field B, Nesbitt LP, Munkley D, Maloney J, Dreyer J, Toohey LL, Campeau T, Dagnone E, Lyver M. Advanced life support for out-of-hospital respiratory distress. New England Journal of Medicine. 2007 May 24;356(21):2156-64.
3. Bickley L, Szilagyi PG. Bates’ guide to physical examination and history-taking. Lippincott Williams & Wilkins; 2012 Nov 1.
Dr. Christopher McLaughlin is a chief resident in the Department of General Surgery at Penn State Hershey Medical Center in Hershey, PA. He obtained his NRP though Good Fellowship Ambulance Company in West Chester, PA, his BS in Biochemistry from Boston College, in Boston, MA, and his MD from Virginia Tech Carilion School of Medicine in Roanoke, VA. His interests include trauma systems, rural EMS, trauma-induced coagulopathy, and prehospital management of chest trauma.


