For this month, we have a case to discuss. The patient in this “case review” is fictional, but the maneuvers and numbers do closely resemble hundreds of cases that were transported during 2020 and 2021 because of COVID ARDS.
The intent of this review is to highlight a moment in time when a flight paramedic learns to abandon a “copy and paste” strategy for transporting patients receiving mechanical ventilatory support and adopt a deliberate, calculated approach for each unique individual. For the seasoned veteran, this will likely seem quite vanilla, but this one is for the new critical care transport clinician.
Case Presentation
The patient is a 24-year-old male, 6’2”, weighing 100kg/IBW 78kg, presenting with ARDS from a confirmed COVID-19 infection. He had a typical initial presentation of shortness of breath and flu-like symptoms but began to rapidly progress to the degree that he required intubation and mechanical ventilation. The outside hospital requested critical care transport for evaluation for ECMO support.
The team arrives at the bedside on hospital day #5 and finds the patient intubated with an 8.0 ET tube (23 @ the lips); ventilator (settings below); 20ga IV in the left AC; 20ga IV in the L forearm; and a foley catheter.
He is receiving propofol at 50mcg/kg/min and is on a fentanyl infusion at 200mcg/hr for pain control and sedation. The sending team communicates some concern that the patient has been “impossible” to keep sedated and that the sending MD has ordered paralysis for transport.
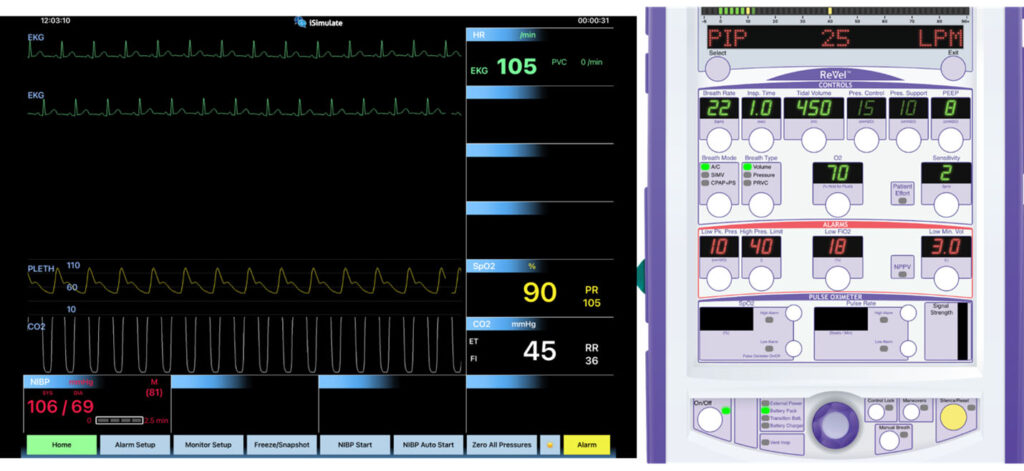
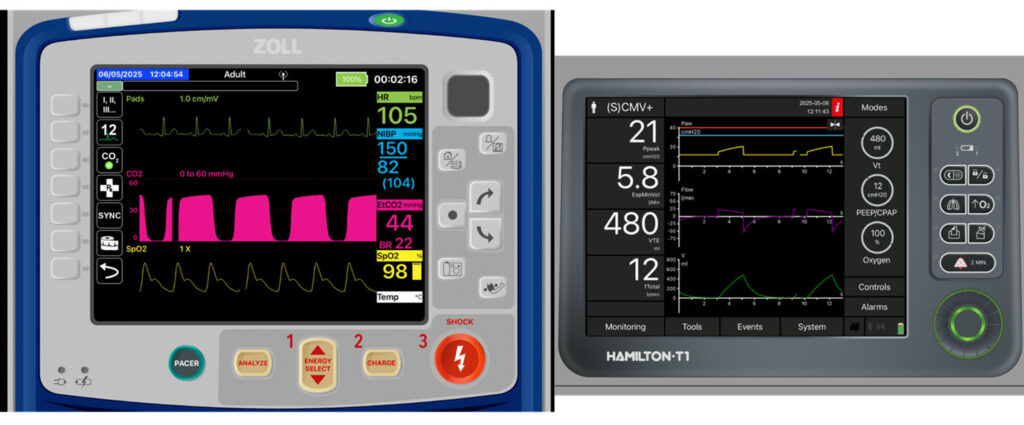
Images provided by the author.
The critical care transport (CCT) team’s first assessment is that the patient is over breathing the set rate on the ventilator by more than 10 breaths per minute. Hemodynamics seem stable; however, the patient is in danger of self-extubating.
A ketamine bolus was administered without the desired effect. The sending physician requested that the patient be reparalyzed for transport to protect the tube. After paralysis, the patient is switched over to the CCT team’s equipment and the team makes a few ventilator changes. Notably the rate, tidal volume and his FiO2.
Now we must ask questions: What was the team doing? Who are they to make changes to the established care? Why were the changes needed?
For the New Clinician
Vented patients are a “bread-and-butter” operation for critical care transport teams. They range in complexity, from simply ventilating and oxygenating the patient, to attempting to recruit alveoli and overcome ARDS to keep the patient alive. In one university level CCT system, ventilated patients accounted for 27% of all transports.1
Of those transports, 50.4% required some type of adjustment or titration en route to the destination facility.1 In another study of a similar type of CCT system, there were over 455 ventilator titrations/maneuvers performed for 237 patients.2 The point being, ventilator titrations in transport are quite common, and simply copying what the sending facility was doing may not be the best strategy.
Sometimes the adjustments are minor tweaks of a respiratory rate to improve ETCo2 management, or a little more volume to overcome a small dead space issue. Sometimes CCT teams must start completely over and ensure that the settings are delivering the appropriate minute volume while protecting against injury.
This typically means ensuring that the tidal volume is calculated based on ideal body weight (for which you will need the patient’s height), not actual weight. That weight is then calculated in the formula 6-8cc/kg (IBW) to obtain the lung protective tidal volume.
Lung protection extends past ensuring safe tidal volumes. Providing a patient the appropriate tidal volume at an inappropriate respiratory rate can be injurious as well. Too fast of a rate increases dead space, reducing the amount of volume that reaches the alveoli.
A fast rate also has to be accounted for with the inspiratory/expiratory ratio (also known as I:E ratio). There has to be adequate cycle time to allow for inspiration and inflation of the alveoli and enough time to completely exhale. Failing to do so can result in hypoventilation, or worse, over-ventilation and air-trapping/auto-PEEP. Emerging evidence, most of which still requires more robust RCT studies, indicates that controlling the respiratory rate is a key element in keeping the overall power or force of ventilation low; this is the key to the prevention of VILI and ARDS.4-6
What You Do Matters
What the transport team does for the patient prior to arrival at the receiving facility dictates what the receiving team can do for the patient.3,7 It is crucial to know when to change the settings that a patient is receiving.
It is not enough to just copy what the sending facility has for vent settings and apply them to the transport vent; there are often many optimizations that need to be made to ensure safe transport for the patient.
Why? One study by Roginski et al. identified that patients who were receiving a high tidal volume in transport were more likely to receive high tidal volumes—in some cases up to 6-12 more hours.3
This means that if the ventilator settings are inappropriate, a patient is potentially being exposed to injurious tidal volume settings for a period of time beyond what is needed to damage the lungs and allow for the formation of ARDS and subsequent damage. Conversely, Stolze et al demonstrated that patients who receive low tidal volumes in air medical transport were more likely to receive low tidal volumes in the ICU.7
Roginski and Stolze demonstrate the vital role of the transport team and how their integration, application physiology and evidence-based practice can create “therapeutic momentum” and sustain the hard-won progress made throughout the patient’s encounter.
A Simple Approach
Titrations like increasing FiO2, decreasing tidal volume and increasing PEEP are common (and simple) adjustments made by CCT teams.2 It is not uncommon to arrive at the bedside of a patient who is “failing” their conventional settings when they have not been optimized. Simple approaches are key.
Ensuring tidal volumes are lung protective and based on ideal body weight; ensuring Fio2 is optimized when Spo2 is persistently low; and titrating PEEP to ensure adequate alveolar recruitment are maneuvers a critical care transport clinician must know how to do.
These maneuvers, supplemented by careful attention to respiratory rate and other respiratory mechanics, can prevent the delivery of safe settings at such a high mechanical power that would limit the protection of those settings.4-6
The Critical Role of Ventilation
On the surface, it seems easier to execute and justify copying the settings that the sending facility was using and plug them in to the transport ventilator. But this mindset neglects the positive impact some simple adjustments and titrations may have on the patient’s overall outcome.
The actions taken during the transport can either build the momentum that the ICU staff can use to focus on other aspects of care, or it can cause friction and inertia that will stall things until the ventilator strategy can be optimized.
More from the Author
Undifferentiated Respiratory Distress: A Medic’s Guide (Part 1)
Undifferentiated Respiratory Distress: A Medic’s Guide (Part 2)
Ventilation Strategies for the Hemodynamically Fragile
Prioritizing Resources: PACE Yourself
References
1. Tran QK, Famuyiwa O, Haase DJ, Holland K, Lawner B, Matta S, McGuin L, Menaker J, Menne A, Ngono EE, Niles E, O’Connor J, Scalea T, Galvagno S. Care Intensity During Transport to the Critical Care Resuscitation Unit: Transport Clinician’s Role. Air Med J. 2020 Nov-Dec;39(6):473-478. doi: 10.1016/j.amj.2020.08.005. Epub 2020 Aug 25. PMID: 33228897.
2. Wilcox SR, Saia MS, Waden H, Frakes M, Wedel SK, Richards JB. Mechanical Ventilation in Critical Care Transport. Air Med J. 2016 May-Jun;35(3):161-5. doi: 10.1016/j.amj.2016.01.004. Epub 2016 Mar 30. PMID: 27255879.
3. Roginski MA, Burney CP, Husson EG, Harper KR, Atchinson PRA, Munson JC. Influence of Critical Care Transport Ventilator Management on Intensive Care Unit Care. Air Med J. 2022 Jan-Feb;41(1):96-102. doi: 10.1016/j.amj.2021.10.005. Epub 2021 Nov 20. PMID: 35248352.
4. Paudel R, Trinkle CA, Waters CM, Robinson LE, Cassity E, Sturgill JL, Broaddus R, Morris PE. Mechanical Power: A New Concept in Mechanical Ventilation. Am J Med Sci. 2021 Dec;362(6):537-545. doi: 10.1016/j.amjms.2021.09.004. Epub 2021 Sep 28. PMID: 34597688; PMCID: PMC8688297.
5. Costa ELV, Slutsky AS, Brochard LJ, Brower R, Serpa-Neto A, Cavalcanti AB, Mercat A, Meade M, Morais CCA, Goligher E, Carvalho CRR, Amato MBP. Ventilatory Variables and Mechanical Power in Patients with Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2021 Aug 1;204(3):303-311. doi: 10.1164/rccm.202009-3467OC. PMID: 33784486.
6. Buiteman-Kruizinga LA, van Meenen DMP, Serpa Neto A, Mazzinari G, Bos LDJ, van der Heiden PLJ, Paulus F, Schultz MJ; NEBULAE; PReVENT; RELAx; investigators. Association of ventilation volumes, pressures and rates with the mechanical power of ventilation in patients without acute respiratory distress syndrome: exploring the impact of rate reduction. Anaesthesia. 2025 May;80(5):533-542. doi: 10.1111/anae.16537. Epub 2025 Jan 13. PMID: 39938476; PMCID: PMC11987796.
7. Stoltze AJ, Wong TS, Harland KK, Ahmed A, Fuller BM, Mohr NM. Prehospital tidal volume influences hospital tidal volume: A cohort study. J Crit Care. 2015 Jun;30(3):495-501. doi: 10.1016/j.jcrc.2015.02.013. Epub 2015 Mar 3. PMID: 25813548; PMCID: PMC4414869.
Cody Winniford is a flight paramedic and base manager in Baltimore, MD. He has a passion for sharing his professional experience in EMS and management. Cody’s clinical and leadership development background spans both military and civilian settings and has served in several capacities as a leader and prehospital clinician. He specializes in air medical and critical care transport, as well as organizational development and leadership development. He is an active speaker on various leadership and clinical topics and is an established and successful educator for prehospital clinicians of all levels. He has a passion for human performance improvement and the mental health and performance aspects of prehospital care.


