
The first OPA was made of metal (left) and was introduced in 1912 by Dr. Joseph Lombard. The Guedel rubber OPA (center) was introduced in 1933. The plastic Berman oral airway (right) was introduced in 1952. Photos courtesy Wood Library-Museum of Anesthesiology and Joseph Hopple
The History of the OPA
My interest in the history of this device began after exploring an old firehouse and finding an antique resuscitator. In its case, clipped to the lid, I found a rusty metal cage that had the unmistakable shape of the OPA.
A little research revealed that the OPA has evolved into what we used today. The airway I found was an example of a Lumbard & Miller airway first introduced by Dr. Joseph Lumbard in 1912 and modified slightly by Dr. Albert Miller in 1918. It was described as a “tongue controller” by Lumbard. I can’t think of a better explanation for the function of the OPA.
The modern OPA is traced back to Dr. Arthur Guedel, who in 1933, introduced the rubber OPA with a single channel in the center. This airway replaced the metal cage airway which was obviously much safer for the patient. Another OPA in use today is the Berman oral airway that was patented by Dr. Robert Berman in 1952. It was plastic in construction and featured a channel on each side to prevent obstruction.

Measure the OPA by placing the top at the patient’s incisor teeth with the tip at the mandibular angle. Photo Joseph Hopple
Gain Control of the Tongue
The OPA has a long history of helping clinicians do the most basic of airway functions: control the tongue. However, it’s not the first step in gaining control, nor can it do it alone after it’s properly inserted.
The OPA is accurately called an airway adjunct, which the Merriam Webster dictionary defines as “something joined or added to another thing but not essentially a part of it.” The essential function is to manually control the tongue with either the head tilt chin lift maneuver or the modified jaw thrust. The OPA adds to or enhances the effectiveness of the manual maneuver, allowing either assisted ventilations or the patient’s own ventilatory efforts. Hence, the OPA alone will not maintain the patent airway that your patient needs, it must be used in concert with good basic airway maneuvers.
Ready to Use
As with any tool in our EMS bag, preparation of the OPA is essential for effective deployment. The OPA is almost always naturally used with the bag-valve Mask (BVM), and having the two in close proximity is paramount to their harmonious use on any patient.
“Out of sight out of mind” is very true in any critical situation. Positioning the OPA near the BVM in both portable kits and inside EMS units helps to enhance the use of both.

Color coding OPAs according to their size can help aid in speeding up the sizing procedure. Photo courtesy Joseph Hopple
Size Matters in Airways
We are taught from the very beginning of our EMS career how to size the OPA. However, as we progress to more advanced airways, this very important step can be rushed or completely forgotten.
If the airway is too small, it can be ineffective as an adjunct or even become a foreign body obstruction in the airway. If the OPA is too large, it can intrude into the glottic opening and obstruct the airway as well.
The most accurate measurement of the OPA is to place the top at patient incisor teeth with the tip at the mandibular angle. Studies have shown this allows the OPA to be its most effective as an adjunct.2
Modern OPAs can be purchased in color coding to help aid in the sizing procedure. Airways that are all white in color can blend together in a large kit, making visual sizing difficult and time consuming.
Insertion of the Airway
Once the proper size is selected the method of insertion can be accomplished using several techniques. The simplest method is to rotate the sized OPA 180 degrees, sliding the tip down the hard palate until you reach the soft palate, then rotate the airway in place behind the tongue.
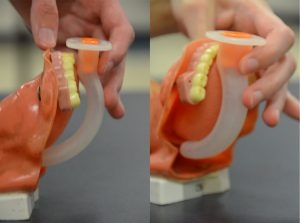
Proper positioning of an OPA will allow it to do its primary function: controlling the tongue. Photo Joseph Hopple
This works well in many patients but can be difficult in a patient with a large tongue. Again, this can be enhanced with good manual positioning of the airway. Using a tongue blade to lift the tongue and the jaw can allow the airway to slip into proper position. Following insertion, be sure to maintain the manual airway position to let the OPA work most effectively.
Conclusion
The OPA is the first airway any EMS provider is educated to use. Reviewing and remembering its history and the simple steps of its use will continue to make it an effective airway for your patient.
Reference
- Effective use of oropharyngeal and nasopharyngeal airways. (n.d.) ACLS Certification Institute. Retrieved May 1, 2019, from www.acls.com/free-resources/knowledge-base/respiratory-arrest-airway-management/nasopharyngeal-oropharyngeal-airways.
Joseph P. Hopple, NRP, is the former education coordinator for Sussex County EMS and is currently the director of emergency services for Old Lycoming Township in Williamsport, Pa, where he also serves on the faculty of the Pennsylvania College of Technology Paramedic program.


