On the go? Listen to the article in the player below!

Non-invasive ventilation will only be effective if your patient is comfortable and you have a good seal with the patient’s face. Photos courtesy Joseph Hopple
When applying a device to deliver noninvasive ventilation (e.g., CPAP or BiPAP) to a patient, many providers forget to pay attention to one of the most critical aspects of using these lifesaving devices: the mask that assists to deliver oxygen at the flow rate set on the device. Remember, the patient’s only interface with the device is through the mask that sits on their face and is essential to the therapy’s success. Taking some time to understand the best practices in mask application will ultimately benefit your patient and improve the treatments success.
Check Your Equipment
As with many procedures in our field, preparation is important to success. This preparation starts long before you contact the patient, it begins at equipment check. Resist the temptation to just “check the box” that your noninvasive ventilation device is present. Inspect it and your mask to be sure its present, not broken and ready to use. Even a disposable unit can be inspected through the package to ensure its readiness.
Comfort the Patient
Upon approaching the patient who you’ve determined will benefit from noninvasive ventilation, preparing them will make the process smoother. Talking calmly with a smooth professional voice will help calm the anxious, shortness of breath patient. Many of our patients have chronic conditions that cause them to either use the noninvasive ventilation at home or have used it before in a crisis. If the patient has a mask at home, look at it as it might help you select the proper size mask if your device has multiple choices.
Ensure Accurate EtCO2 Reading
One important preparation is the application of EtCO2 monitoring to your patient. Studies have shown that the nasal cannula monitor gives the most accurate reading during use.1,2 The way the mask seal works will allow it to obtain its seal with the nasal cannula in place. If you’re an ALS service, a good practice is to place a cannula with your device to prompt its application. If you’re a BLS user of CPAP, and don’t use EtCO2 monitoring, work with your ALS provider to obtain a cannula to put with your CPAP so it’s applied and ready when ALS arrives. This prevents the mask seal being disturbed to apply EtCO2 when ALS arrives.
Use the Right Mask to Ensure the Right Fit
Good preparation has helped you efficiently get to the application process. Using the Pulmodyne Bitrac ED mask as an example, the medium mask that comes packed with the unit will fit 85% of the adult patient population.
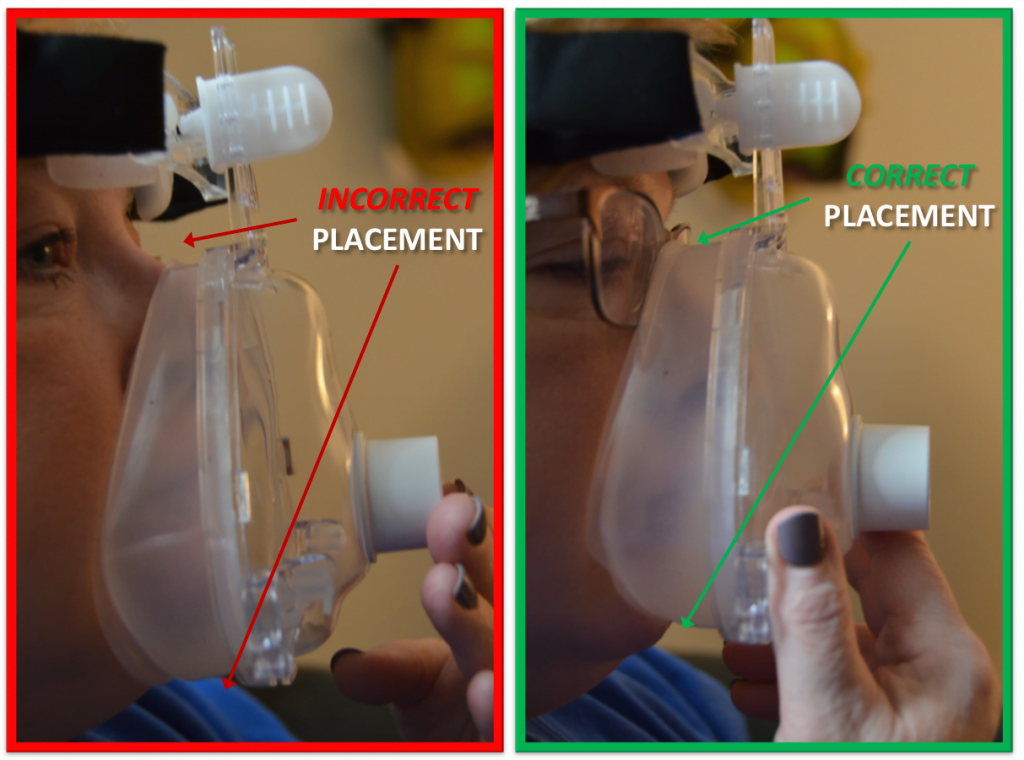
Figure 1: Placement of the mask to ensure proper fit
Look at the mask and then look at your patient to judge size. The apex or top of the mask should sit at the level you would expect eyeglasses to sit. The bottom should rest just below the bottom lip. A mistake many providers make is thinking the bottom on the mask is a “chin cup.” This will lead to an uncomfortable fit for the patient and difficulty obtaining a seal. (See Figure 1.)
Many agencies keep a large mask available for the limited patient population that the medium mask will not fit. You should resist the “one size fits all” attitude, because it doesn’t help your patients.
Prepare the Patient
Calm and supportive, positive reinforcement is now essential as the application process proceeds. Start the device and have the patient hold the mask to their face to get used to the feel. If you have a patient who has never used a device for noninvasive ventilation before, and you’re applying CPAP, a good example to give them is the feeling of a brisk wind in their face or holding their head out of a moving vehicle. Starting the air flowing also fills the duel lip cushion with air allowing it to obtain a seal with very little pressure.

Figure 2: Securing the mask on the patient and making adjustments
Secure the Mask
Once the patient is comfortable and you have obtained a soft seal, you can then secure the mask with the head straps. Adjust the forehead pad to fit against the patient’s forehead keeping the mask in place. Work the head straps down to rest comfortably with the back on the occipital area and clip the straps to the mask. Adjust both sides simultaneously, gently, but not too tight. If you overtighten the mask you may lose the seal. If you do have a leak, try to loosen the straps then check the seal. (See Figure 2.)
Conclusion
Using a device to deliver noninvasive ventilation will only be effective if your patient is comfortable and you have a good seal with the patients face. Taking some time to prepare yourself, your equipment and your patient will increase your success with this life changing therapy.
References
- Nuccio P, Hochstetler G, Jackson M. End-tidal CO2 measurements with noninvasive ventilation. Anesth Analg. 2007;105(S 6):111. (Download here.)
- Wesley K. Pump Problems: EMS providers use capnography to monitor CHF. JEMS. 2012;37(3 Suppl):8–11.
Joseph P. Hopple, NRP, is the former education coordinator for Sussex County EMS and is currently the director of emergency services for Old Lycoming Township in Williamsport, Pa, where he also serves on the faculty of the Pennsylvania College of Technology Paramedic program.



Recent Comments